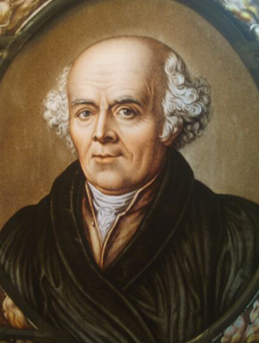
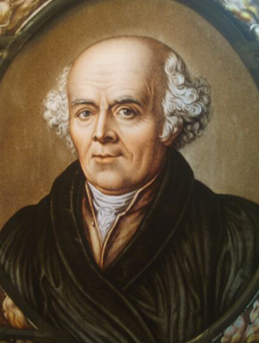
OUR GREAT MASTER Dr CHRISTIANFRIEDRICH SAMUEL HAHNEMANN (1755-1843)
Homoeopathy was discovered by German Physician, Dr. Christian Friedrich Samuel Hahnemann (1755-1843), in the late eighteenth century. Homoeopathy is a therapeutic system of medicine premised on the principle, "Similia Similibus Curentur" or 'let likes be treated by likes'. Homoeopathy is a method of treatment for curing the patient by medicines that possess the power of producing similar symptoms in a healthy human being simulating the natural disease, which it can cure in the diseased person. Homoeopathy treats the patients not only through holistic approach but also considers individualistic characteristics of the person. This concept of 'law of similars' was also enunciated by Hippocrates and Paracelsus, but Dr. Hahnemann established it on a scientific footing despite the fact that he lived in an age when modern laboratory methods were almost unknown.
Homoeopathic medicines are prepared from traces of animal, plant, mineral and other natural substances, by a standard method called dynamisation or potentisation, which comprises of successive dilutions and succussions to raise the inherent curative power of the drugs to maximum. The medicines thus prepared through 'potentisation', attain their potential enhanced enormously to combat ailments while at the same time absence of toxicity is assured. The medicines are usually proved in healthy human beings, to ascertain their curative properties. The system believes in the existence of a regulating force (Vital Force) in the organism, which plays a vital role during health, disease and cure. The symptoms are considered as the body's natural reaction to the illness and help to find a remedy against the illness. The remedies work by stimulating the body's defense mechanism to correct itself naturally. This therapy adopts an individualistic and holistic approach towards the sick individual. A homoeopathic doctor does not treat in the name of disease, rather the treatment is targeted against the "patient" who is suffering from a particular disease. The physician perceives all the derangements at physical and mental levels of the patient, brings about conceptual image of the patient through totality of symptoms and selects the medicine, which is most similar to the picture of the patient. Thus the dictum goes " Homoeopathy treats the patient, and not the disease". Homoeopathic medicines are most cost effective, palatable, have no adverse side effects, can be administered easily. In some cases, the medicines can be prescribed on the basis of symptoms of the patients, without depending upon the cumbersome and costly diagnostic modalities.
Homoeopathy has been useful in treatment of psychosomatic disorders, autoimmune diseases, geriatric and pediatric disorders, ailments during pregnancy, obstinate skin diseases, life style disorders and allergies, etc. It also has a positive role in improving the quality of life in incurable chronic diseases like cancer, HIV/AIDS, terminally ill patients and incapacitating diseases like rheumatoid arthritis, etc.
A novel coronavirus (COVID-19) was identified in 2019 in Wuhan, China. This is a new coronavirus that has not been previously identified in humans. China first reported this outbreak to the World Health Organization on December 31, 2019. Since then, scientific reports have emerged suggesting the disease likely began spreading several months earlier, sometime last fall. Either way, this means that in just the span of a few months, the virus has infected at least 28,000 people in China and spread around the world. That's an unusually rapid rise for a brand new virus when we consider the draconian measures China has taken to control the virus, including an unprecedented quarantine of more than 50 million people.The evidence is highly suggestive that the outbreak is associated with exposures in one seafood market in wuhan.
Epidemology Coronaviruses (CoV) are single-stranded positive-sense RNA viruses that infect animals and humans. These are classified into 4 genera based on their host specificity: Alphacoronavirus, Betacoronavirus, Deltacoronavirus and Gamma Coronavirus. There are seven known types of CoVs that include 229E and NL63 (Genus Alphacoronavirus), OC43, HKU1, MERS and SARS (Genus Betacoronavirus). While 229E, NL63, OC43, and HKU1 commonly infect humans.
The SARS and MERS outbreak in 2002 and 2012 respectively occurred when the virus crossed-over from animals to humans causing significant mortality ). In December 2019, another outbreak of coronavirus was reported from Wuhan, China that also transmitted from animals to humans. This new virus has been temporarily termed as 2019-novel Coronavirus (2019-nCoV) by the World Health Organization (WHO) .While there are several hypotheses about the origin of 2019-nCoV, the source of this ongoing outbreak remains elusive TRANSMISSION Coronaviruses are zoonotic. This means they first develop in animals before developing in humans. For the virus to pass from animal to humans, a person has to come into close contact with an animal that carries the infection. Once the virus develops in people, coronaviruses can be spread from person to person through as follows ● Between people who are in close contact with one another. ● Through respiratory droplets moves through the air when you cough or sneeze. The viral material hangs out in these droplets and can be breathed into the respiratory tract (your windpipe and lungs), where the virus can then lead to an infection. The 2019 coronavirus hasn't been definitively linked to a specific animal.But researchers believe that the virus may have been passed from bats to another animal — either snakes or pangolins — and then transmitted to humans. This transmission likely occurred in the open food market in Wuhan, China.Virus first isolated from a patient with atypical pneumonia. Symptoms
Signs and symptoms of coronavirus disease 2019 (COVID-19) may appear 2 to 14 days after exposure. This time after exposure and before having symptoms is called the incubation period. You can still spread COVID-19 before you have symptoms (presymptomatic transmission). Common signs and symptoms can include:
• Fever
• Cough
• Tiredness
Early symptoms of COVID-19 may include a loss of taste or smell.
Other symptoms can include:
• Shortness of breath or difficulty breathing
• Muscle aches
• Chills
• Sore throat
• Runny nose
• Headache
• Chest pain
• Pink eye (conjunctivitis)
• Nausea
• Vomiting
• Diarrhea
• Rash
The severity of COVID-19 symptoms can range from very mild to severe. Some people may have only a few symptoms. Some people may have no symptoms at all, but can still spread it (asymptomatic transmission). Some people may experience worsened symptoms, such as worsened shortness of breath and pneumonia, about a week after symptoms start.
Some people experience COVID-19 symptoms for more than four weeks after they're diagnosed. These health issues are sometimes called post-COVID-19 conditions. Some children experience multisystem inflammatory syndrome, a syndrome that can affect some organs and tissues, several weeks after having COVID-19. Rarely, some adults experience the syndrome too.People who are older have a higher risk of serious illness from COVID-19, and the risk increases with age. People who have existing medical conditions also may have a higher risk of serious illness. Certain medical conditions that may increase the risk of serious
The emergence of the coronavirus disease 2019 (COVID-19), which is caused by infection from the previously unknown severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has devastated economies and caused unprecedented challenges to healthcare and food systems around the world. Globally, billions of people have been ordered to stay at home as a result of lockdowns, while almost three million people have died (as of the end of March 2021).
The most commonly reported symptoms of post-COVID-19 syndrome include:
• Fatigue
• Symptoms that get worse after physical or mental effort
• Fever
• Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
• Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
• Joint or muscle pain
• Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
• Digestive symptoms, including diarrhea and stomach pain
• Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
• Other symptoms, such as a rash and changes in the menstrual cycle
The Global Health Security (GHS) Index At the end of the Ebola outbreak that occurred in 2014, the GHS Index was developed to determine the ability of a total of 195 countries to cope with a future infectious disease outbreak. In order to make this prediction, the GHS Index considers the biological risks of each country, which includes an analysis of the nation's current geopolitics, health system and capacity to control infectious disease outbreaks.To evaluate a given country's GHS Index, they are rated on prevention, detection andreporting, rapid response, health system, compliance with international norms and risk environment.Since the outbreak of COVID-19, public health officials have investigated whether the GHS Index could be used to assess the performance of countries during the current pandemic. In a research study looking to do just this, the GHS Index was found to have a positive correlation with COVID-19 associated morbidity and mortality rates in 178 different countries.
The effect of COVID-19 on other health problems
The COVID-19 pandemic has overwhelmed healthcare systems around the world, having a knock-on effect on the diagnosis and treatment of other diseases.Social distancing and lockdowns have reduced diagnosis rates of infectious diseases suchas seasonal influenza, as would be expected with reduced social contact.
However, individuals have avoided seeking help for other health problems due to lockdowns and avoidance of medical settings, leading to reduced diagnosis and treatment despite the problem still being there. Meanwhile, even in diagnosed cases, treatment for diseases and conditions such as cancer had to be postponed in many cases due to the immediate threat of COVID-19 consuming health systems and their resources.Scientific research around the world has also focused on COVID-19, potentially delaying research and breakthroughs on other diseases.
Furthermore, other infectious diseases such as malaria, HIV and tuberculosis were put on the sidelines, despite still being very real problems, particularly in more vulnerable populations. An assessment by the Bill & Melinda Gates foundations in September 2020 assessed data on vaccine coverage from the first portion of the pandemic and came to a conclusion that vaccine coverage in health systems had been pushed back around 25years in 25 weeks.Before the pandemic, around half of the world's population did not have access to essential healthcare, and this number has been increased by the pandemic. Healthcare systems across the globe need to become more accessible and need to be prepared for future pandemic-like events in a way that will reduce the impact on the management of other diseases.
Obesity is a complex disease involving an excessive amount of body fat. Obesity isn't just a cosmetic concern. It's a medical problem that increases the risk of other diseases and health problems, such as heart disease, diabetes, high blood pressure and certain cancers.
Obesity is an alarmingly increasing global public health issue. Several countries worldwide have witnessed a double or triple escalation in the prevalence of obesity in the last three decades, probably due to urbanization, sedentary lifestyle, and increase consumption of high-calorie processed food. The alarming increase in childhood obesity foreshows a tremendous burden of chronic disease prevention in the future public healthcare systems worldwide. Obesity prevention is a critical factor in controlling Obesity-related Non-communicable diseases (OR-NCDs), including diabetes, cardiovascular disease, stroke, hypertension, cancer, and psychological problems. This activity reviews the public health considerations in obesity and highlights the role of the interprofessional team in developing public health strategies for the management and prevention of this condition.
The failure of the traditional obesity control measures has stressed the importance of a new non-stigmatizing public policy approach, shifting away from the traditional focus on individual behavior change towards strategies dealing with environmental change. The other big challenge related to overweight and obesity is weight bias and discrimination. In public settings such as work environments, healthcare facilities, and educational setup, obese individuals face discrimination.
PREVALANCE
According to the World Health Organisation (2016), there are around 2 billion adults currently living with overweight, of which 650 million are considered to be affected by obesity (BMI ≥30 kg/m²). That equates to 39% (39% of men and 40% of women) of adults aged 18 or over living with overweight and 13% living with obesity. It is now estimated that most of the world's population lives in countries where overweight and obesity is a bigger risk to health than underweight.Public Health Impact of Obesity
Life expectancy: Obesity, the modern lifestyle disease, not only cause serious illness but also substantially decreases the average public life expectancy. Obesity in adulthood is a strong predictor of early death. Framingham Heart Study, a prospective cohort study, revealed that adults who were obese at 40 years lost 6 to 7 years of expected life. However, in obese people who smoked, the years of life lost almost doubled.
Quality of life: Obesity affects both the physical and psychosocial aspects of quality of life, more significant among morbidly obese individuals. The self-perceived Health-related quality of life (HRQL) among obese individuals worsens with increasing BMI. The effect of obesity on HRQL is assessed most frequently by SF-36 (Short-Form Health Survey), comprising 36 questions covering eight domains including physical functioning, physical role limitations due to physical health problems, social functioning, bodily pain, general mental well being, emotional role limitations, energy, and general health perceptions] The risk of suffering from any chronic medical condition is almost doubled in morbid obesity compared to overweight individuals. Obesity causes a substantial psychological burden exacerbated by the public's marked preoccupation with thinness. Sullivan et al. reported more significant psychosocial consequences in obese women when compared to obese men.
Prevalence of obesity-associated diseases: The individuals who are obese in their childhood tend to remain obese in adulthood and prone to high risk for Obesity-related non-communicable diseases (OR-NCD) at a younger age.[12] Obesity-related non-communicable diseases, including type 2 diabetes, coronary heart disease, stroke, cancer, asthma, and chronic obstructive pulmonary disease, have increased worldwide. These non-communicable diseases are primary targets for global disease prevention by WHO. Compared with their normal-weight peers, severely obese individuals lose about eight disease-free years, and mildly obese individuals lose about four disease-free years.EMPLoyment: Obesity is one of the leading reasons for discrimination in the hiring process for employment, more noticed among obese females than obese males. Obesity can cause reduced employment and an increase in self-reported work limitations compared to normal-weight individuals.
Economic impact: Obesity is estimated to account for more than 20% of all annual health care expenditures in the United States. The medical costs are 30% to 40% higher among obese individuals than their normal-weight peers, double the increase attributable to smoking.[he direct costs of obesity are attributed to the amount spent on diagnosing and treating obesity and obesity-related chronic comorbid conditions such as cardiovascular disease and type 2 diabetes. Indirect costs are attributed to the lost wages secondary to illness and premature death, elevated costs paid for disability and insurance claims, and decreased productivity at work.
Clinical Significance
The World Health Organization describes obesity as an excessive fat accumulation with body mass index (BMI) ≥25 kg/m2 labeled as overweight and BMI ≥ 30 kg/m2 labeled obesity. The relative risk of death increases with an increase in BMI. This association is non-linear, with a much higher relative risk of death for very high BMI (>30) individuals.[19] The stigma of obesity is a threat to proper healthcare resource utilization, preventing morbidity, and identifying complications early. Obese individuals have lower rates of age-appropriate preventive cancer screening Women who suffer from obesity delay seeking routine gynecological cancer screening due to many social barriers] The compromise in healthcare quality in obese individuals adds to the burden of morbidity and all-cause mortality; This also imposes a significant load on the healthcare system in managing comorbidities of obese individuals. Crucial risk factors have been recognized in several studies as an effort to decrease the obesity burden, which includes the perinatal factors like maternal antenatal BMI, weight at birth and child's nutrition in the first three years of life, feeding options (breastfeeding versus formula feeding), and growth pattern in the first year The FDA has officially banned trans fats in all foods sold in restaurants and grocery stores.Obesity prevention priorities should focus more on children, particularly in schools encouraging healthy habits. The local government should restrict commercial permits for fast-food restaurants nearby schools (within 0.5 miles) and encourage healthy food vendors to establish near schools.School-level policies should improve physical education at school and encourage walking or biking to school.Levying significant tax for unhealthy food and subsidizing healthy food are crucial strategies to prevent obesity but with few ethical limitations. Taxes on sugar-sweetened beverages such as soft drinks have been applied at most state and city levels.Public health policy should focus on designing activity-friendly communities by creating bike and walking paths.
Family-Based Interventions
The family-based approach is the best intervention to sustain weight loss and have weight maintenance among patients with overweight or obesity. The overweight subjects living in a family will have significant difficulties changing their lifestyle without family support. Several studies have proven that a low-fat diet with high protein and a low glycemic index effectively sustains weight maintenance and weight regain.[An easy-to-use tool in family-based dietary intervention is the traffic light diet in which food is classified as green, red, and yellowWeight Bias in Health Care The weight bias in the health care system can be explicit (consciously expressed) or implicit (involuntarily expressed). Implicit weight bias is not rare to see among Health care providers. Society's negative biases towards overweight or obesity often are shared and exhibited by the health care provider (HCP). The weight bias by the health care team can impair the patient's health care quality. Most HCPs believe in the energy balance theory of weight control, which encourages the thinking of obesity issues being a personal responsibility and limiting the scope of appropriate counseling.
The following interventions could help in reducing the weight bias in health practice.
• To educate the health care professionals about the complex etiology of obesity, including genetic, metabolic, and social factors.
• To make providers aware of the fact that the weight bias could influence the quality of the care.
• To train the medical trainees how to communicate without implicit bias.
Another strategy is to expose counter-stereotypical exemplars of people with obesity who are successful and intelligent.
• HCPs should address the overall health and the patient's understanding of obesity-associated comorbidities along with weight loss management.
• HCPs should be encouraged to use people-first language, e.g., patients with obesity instead of obese patients. Also, using terminology like high BMI instead of morbid obesity will help in motivating the patient.
Obesity is a national epidemic affecting every one in three adults and one in six children in the United States of America. The rising trend has been attributed to change in environmental and food practices in the face of the increasingly sedentary lifestyles of people. Tracking childhood obesity into adulthood poses a significant burden on the healthcare system for managing this and its complications.
Obesity is crucial to developing non-communicable diseases (OR-NCD), which include diabetes,hypertension, coronary artery diseases, to name a few. The psychological aspect regarding the stigma of obesity leads to delay in seeking healthcare in these individuals.
While the primary care physician diagnoses obesity, it is equally important to consult with an interprofessional team of specialists, including dieticians, psychologists, behavioral counselors, and exercise specialists. When managing a child with obesity, consultation with pediatric endocrinologists, neurologists, and surgeons also has a vital role in the child's growth. Nurse practitioners are a vital part of the interprofessional group as continued and frequent motivation is needed to inculcate positive health-related changes in their daily life.
Psychological problems play a significant role in the development of maladaptive eating patterns in children and adults. The role of behavioral counselors and school-based health groups in managing children with obesity is crucial. The role of public health policymakers becomes pivotal because obesity is a preventable disease. Coordination between healthcare providers and policymakers, operating as an interprofessional team, is essential to gauge the burden of the disease, address the barriers to seeking treatment and preventive screenings. The failure of the traditional obesity control measures has stressed the importance of developing a new non-stigmatizing public policy approach by public health officials
Alcohol and illicit drug use has a significant impact on global health. Alcohol consumption is increasing worldwide, particularly in developing countries and countries in transition, leading to an increasing number of health and social problems, both acute and chronic. Illicit drug use is also increasing, particularly injection drug use, followed by an epidemic spread of HIV and other blood-borne infections. Alcohol and illicit drug use are related to key determinants of population health and are also an outcome of poor health. Globalized marketing and trade, and rapid social changes and development in the absence of strong policies and investments in public health have led to an increased availability, use and problems related to alcohol and other substance use. Public health policies and substantial investments in effective prevention and treatment approaches are needed in order to reduce the negative impact of alcohol and other drug use at national and global levels.
Use and abuse of drugs and alcohol by teens is very common and can have serious consequences. In the 15-24 year age range, 50% of deaths (from accidents, homicides, suicides) involve alcohol or drug abuse. Drugs and alcohol also contribute to physical and sexual aggression such as assault or rape. Possible stages of teenage experience with alcohol and drugs include abstinence (non-use), experimentation, regular use (both recreational and compensatory for other problems), abuse, and dependency. Repeated and regular recreational use can lead to other problems like anxiety and depression. Some teenagers regularly use drugs or alcohol to compensate for anxiety, depression, or a lack of positive social skills. Teen use of tobacco and alcohol should not be minimized because they can be "gateway drugs" for other drugs (marijuana, cocaine, hallucinogens, inhalants, and heroin).
Health Effects of Drug and Alcohol Abuse
The abuse of drugs or alcohol can cause changes to brain chemistry. Further, the substance is often processed through many different body systems, potentially causing wider spread damage. These changes can lead to lasting damage.Infections and Immune System Damage Drugs that are injected intravenously carry a very high risk of infection, especially from HIV, hepatitis B and C, or bacterial infections from sharing dirty needles. Other drugs also increase the risk of certain infections, such as upper respiratory infections from snorting or smoking drugs.
The euphoria associated with many intoxicating substances, especially alcohol, cocaine, and narcotics, can lower inhibitions, which increases the chance of taking sexual risks and contracting an STI. Some drugs, like cocaine, directly impact the immune system's ability to create white blood cells, which reduces immune response to infection.
Experts estimate that around half of all adult patients with pneumonia have abused alcohol in the past. Those with alcohol abuse issues and pneumococcal pneumonia see more severe complications and a higher rate of mortality than pneumonia patients who have not abused alcohol.
Cardiovascular Problems
Stimulants can increase a user's heart rate while CNS depressants can slow it down. Consistent high or low blood pressure may be associated with an increased risk of blood clots, ischemic injury, and other circulatory problems such as aortic or coronary arterial dissection. Many intoxicating substances can cause irregular heartbeat. Stimulants, like cocaine or methamphetamines, can lead to overdose deaths from cardiac arrest.Those who abuse alcohol are at higher risks of:
• Pneumonia.• Tuberculosis.
• Respiratory syncytial virus infection.
• Acute respiratory distress syndrome.
Taking drugs intravenously can also have negative cardiovascular effects, such as local and disseminated vascular inflammation, cardiac valve infections, and otherwise a potential for increased exposure to several bloodborne infectious processes.
Gastrointestinal Issues
Drugs that are ingested orally, such as alcohol or prescription drugs like opioids or ADHD medication can cause harm to the digestive system. Opioids can lead to chronic constipation, and other substances can cause stomach upset, indigestion, nausea, or vomiting. Chronic indigestion (such as that associated with chronic drinking) is called gastrointestinal reflux disease (GERD), which can damage the esophagus and make eating certain foods painful. Frequent, substance-related vomiting can also cause damage to the esophagus and lead to problems with malnutrition.Alcohol abuse is additionally associated with
• Reflux esophagitis.• Increased GI cancer risk.
• Pancreatitis.
• Mallory-Weiss tears (ruptured lower esophagus resulting in GI bleeding).
• Malabsorption and nutritional deficiencies.
Cocaine and methamphetamine use is also associated with some dangerous gastrointestinal issues, such as mesenteric arterial vasospasm, which can lead to a loss of blood supply between the heart and the gastrointestinal system. This can lead to ischemic colitis and, in severe cases, bowel tissue death, known as bowel necrosis.
Respiratory Problems
Smoking any drug can damage alveoli in the lungs and make the upper respiratory system more susceptible to infections.Some CNS depressants, especially opioids, can slow breathing or make breathing shallow or irregular. If a person overdoses on opioids or some other CNS depressants, hypoxia can lead to death; however, if a person has a reduced or depressed breathing pattern for a long time due to addiction, their body could also become starved of oxygen, leading to damage to other organ systems. Chronic alcohol use is associated with an increased risk of community-acquired pneumonia, such as those caused by Streptococcus pneumoniae.
Liver Damage
The liver is involved with nutrient metabolization, but is also a primary site of detoxification for many types of consumed substances. In the face of constantly high levels of certain drugs, the liver can become overwhelmed in its metabolic duties, and the tissues of the organ begin to break down. Alcohol, inhalants, heroin, and steroids can all rapidly damage the liver, causing cirrhosis or hepatitis.Alcohol, especially, can lead to a spectrum of liver disease that ranges from the relatively mild (alcoholic steatohepatitis, known as fatty liver) to more severe inflammation (alcoholic hepatitis) to progressive fibrosis and scarring of the liver parenchyma (cirrhosis). Cirrhosis is itself a risk factor for the development of liver cancer.
Kidney Damage
The kidneys also filter toxins out of the bloodstream, so they are affected by large amounts of any dangerous substance in the blood. Some drugs are associated with a condition known as rhabdomyolysis, which is the breakdown of muscle tissue that floods the bloodstream with toxic levels of muscle cell contents, including a large protein known as myoglobin; as a result, the kidneys may become overwhelmed and unable to filter toxins efficiently.This can result in progressive kidney damage, leading up to renal failure that requires dialysis. Drugs like heroin or other opioids that result in respiratory depression and an associated reduction in the amount of oxygen the body takes in can also cause kidney damage. Also, additives and impurities in some illicit street drugs may also clog the small vessels that supply blood to the kidneys after being injected, resulting in damage to these vital organs.
Neurological Issues
When a person struggles with substance abuse for a long time, the brain adapts. As it does so, certain changes in brain chemistry accompany the development of physical dependence to the substance in question.In addition to physical dependence, consistent use of an addictive substance may ultimately lead to addiction, a brain disorder. As addiction develops, regions of the brain involved with several key functions such as reward/pleasure, decision making, and impulse control, may undergo changes Alcohol, benzodiazepines, and other sedative-hypnotics are central nervous system depressants, meaning they reduce excitatory brain signaling, leading to a greater sense of calm or relaxation. At high enough doses, these drugs are also associated with movement problems, significant cognitive impairment, and memory loss.
Stimulants like cocaine, meth, ecstasy, and some other designer drugs increase neuron firing, leading to greater attention, emotional highs, and physical energy. However, once these drugs begin to leave the body, negative side effects may develop as the brain may be slower to restore balance to neurotransmitters like serotonin, dopamine, and norepinephrine.
Survival chances for adolescents and young adults vary greatly across the world. In 2020, the probability of dying among those aged 10–24 years was highest in sub-Saharan Africa, Oceania (excluding Australia and New Zealand), northern Africa and southern Asia (1). The average global probability of a 10-year-old dying before age 24 was 6 times higher in sub-Saharan Africa than in North America and Europe.
Main health issues
Injuries
Unintentional injuries are the leading cause of death and disability among adolescents. In 2019, nearly 100 000 adolescents (10–19 years) died as a result of road traffic accidents. Many of those who died were vulnerable road users, including pedestrians, cyclists or users of motorized two-wheelers. In many countries, road safety laws need to be made more comprehensive, and enforcement of such laws needs to be strengthened. Furthermore, young drivers need advice on driving safely, while laws that prohibit driving under the influence of alcohol and drugs need to be strictly enforced among all age groups. Blood alcohol levels should be set lower for young drivers than for adults. Graduated licences for novice drivers with zero-tolerance for drink-driving are recommended.Drowning is also among the top causes of death among adolescents; more than 40 000 adolescents, over three quarters of them boys, are estimated to have drowned in 2019. Teaching children and adolescents to swim is an essential intervention to prevent these deaths.
Violence
Interpersonal violence is among the leading causes of death in adolescents and young people globally. Its prominence varies substantially by world region. It causes nearly a third of all adolescent male deaths in low- and middle-income countries in the WHO Region of the Americas. According to the global school-based student health survey 42% of adolescent boys and 37% of adolescent girls were exposed to bullying. Sexual violence also affects a significant proportion of youth: 1 in 8 young people report sexual abuse.Violence during adolescence also increases the risks of injury, HIV and other sexually transmitted infections, mental health problems, poor school performance and dropout, early pregnancy, reproductive health problems, and communicable and noncommunicable diseases.
Effective prevention and response strategies include promoting parenting and early childhood development; addressing school-based bullying prevention, programmes that develop life and social skills, and community approaches to reduce access to alcohol and firearms. Effective and empathetic care for adolescent survivors of violence, including ongoing support, can help with the physical and psychological consequences.
Mental health
Depression is one of the leading causes of illness and disability among adolescents, and suicide is the second leading cause of death in people aged 15–19 years (2). Mental health conditions account for 16% of the global burden of disease and injury in people aged 10–19 years. Half of all mental health disorders in adulthood start by age 14, but most cases are undetected and untreated.Many factors have an impact on the well-being and mental health of adolescents. Violence, poverty, stigma, exclusion, and living in humanitarian and fragile settings can increase the risk of developing mental health problems. The consequences of not addressing adolescent mental health conditions extend to adulthood, impairing both physical and mental health and limiting opportunities to lead fulfilling lives as adults.Building socioemotional skills in children and adolescents and providing them with psychosocial support in schools and other community settings can help promote good mental health. Programmes to help strengthen the ties between adolescents and their families and improve quality of home environments are also important. If problems arise, they should be detected and timely managed by competent and caring health workers.
Alcohol and drug use
Drinking alcohol among adolescents is a major concern in many countries. it can reduce self-control and increase risky behaviours, such as unsafe sex or dangerous driving. It is an underlying cause of injuries (including those due to road traffic accidents), violence and premature deaths. It can also lead to health problems in later life and affects life expectancy. Worldwide, more than a quarter of all people aged 15–19 years are current drinkers, amounting to 155 million adolescents. Prevalence of heavy episodic drinking among adolescents aged 15–19 years was 13.6% in 2016, with males most at risk.Cannabis is the most widely used psychoactive drug among young people with about 4.7% of people aged 15–16 years using it at least once in 2018. Alcohol and drug use in children and adolescents is associated with neurocognitive alterations which can lead to behavioural, emotional, social and academic problems in later life.
Prevention of alcohol and drug use are important areas of public health actions and may include population-based strategies and interventions, activities in school, community, family and on the individual level. Setting a minimum age for buying and consuming alcohol and eliminate marketing and advertising to minors are among the key strategies for reducing drinking among adolescents.
Tobacco use
The vast majority of people using tobacco today began doing so when they were adolescents. Prohibiting the sale of tobacco products to minors (under 18 years) and increasing the price of tobacco products through higher taxes, banning tobacco advertising and ensuring smoke-free environments are crucial. Globally, at least 1 in 10 adolescents aged 13–15 years uses tobacco, although there are areas where this figure is much higher.HIV/AIDS
An estimated 1.7 million adolescents (age 10–19 years) were living with HIV in 2019 with around 90% in the WHO African Region. While there have been substantial declines in new infections amongst adolescents from a peak in 1994, adolescents still account for about 10% of new adult HIV infections, with three-quarters amongst adolescent girls. Additionally, while new infections may have fallen in many of the most severely affected countries, recent testing coverage remains low suggesting that many adolescents and young people living with HIV may not know their status.Adolescents living with HIV have worse access to antiretroviral treatment, adherence to treatment, retention in care and viral suppression. A key factor contributing to these is limited provision of adolescent-friendly services including psychosocial interventions and support.
Adolescents and young people need to know how to protect themselves from HIV infection and must also have the means to do so. This includes being able to obtain access HIV prevention interventions including voluntary medical male circumcision, condoms and pre-exposure prophylaxis, better access to HIV testing and counselling, and stronger links to HIV treatment services for those who test HIV positive.
Other infectious diseases
Thanks to improved childhood vaccination, adolescent deaths and disability from measles have fallen markedly. For example, adolescent mortality from measles fell by 90% in the African Region between 2000 and 2012.Diarrhoea and lower respiratory tract infections (pneumonia) are estimated to be among the top 10 causes of death for adolescents 10–14 years. These two diseases, along with meningitis, are all among the top 5 causes of adolescent death in African low- and middle-income countries.
Infectious diseases like with human papilloma virus that normally occurs after onset of sexual activity can lead to both short-term disease (genital warts) during adolescence but more importantly also leads to cervical and other cancers several decades later. Early adolescence (9–14 years) is the optimal time for vaccination against HPV infection and it is estimated that if 90% of girls globally get the HPV vaccine more than 40 million lives could be saved over the next century. However, it is estimated that in 2019 only 15% of girls globally received the vaccine.
Early pregnancy and childbirth
Approximately 12 million girls aged 15–19 years and at least 777 000 girls under 15 years give birth each year in developing regions. Complications from pregnancy and childbirth are among the leading causes of death for girls aged 15–19 years globally.The UN Population Division puts the global adolescent birth rate in 2020 at 41 births per 1000 girls this age, and country rates range from 1 to over 200 births per 1000 girls . This indicates a marked decrease since 1990. This decrease is reflected in a similar decline in maternal mortality rates among girls aged 15–19 years.One of the specific targets of the health Sustainable Development Goal is that by 2030, the world should ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes.
Adolescents need and have a right to comprehensive sexuality education, a curriculum-based process of teaching and learning about the cognitive, emotional, physical and social aspects of sexuality. Better access to contraceptive information and services can reduce the number of girls becoming pregnant and giving birth at too young an age. Laws that are enforced that specify a minimum age of marriage at 18 can help. Girls who do become pregnant need access to quality antenatal care. Where permitted by law, adolescents who opt to terminate their pregnancies should have access to safe abortion.
Nutrition and micronutrient deficiencies
Iron deficiency anaemia was the second leading cause of years lost by adolescents to death and disability in 2019. Iron and folic acid supplements are a solution that also helps to promote health before adolescents become parents. Regular deworming in areas where intestinal helminths such as hookworm are common is recommended to prevent micronutrient (including iron) deficiencies.Developing healthy eating habits in adolescence are foundations for good health in adulthood. Reducing the marketing of foods high in saturated fats, trans-fatty acids, free sugars, or salt and providing access to healthy foods are important for all, but especially for children and adolescents.
Undernutrition and obesity
Many boys and girls in developing countries enter adolescence undernourished, making them more vulnerable to disease and early death. At the other end of the spectrum, the number of adolescents who are overweight or obese is increasing in low-, middle- and high-income countries.Globally, in 2016, over 1 in 6 adolescents aged 10–19 years was overweight. Prevalence varied across WHO regions, from lower than 10% in the WHO South-East Asia Region to over 30% in the WHO Region of the Americas.
Physical activity
Physical activity provides fundamental health benefits for adolescents, including improved cardiorespiratory and muscular fitness, bone health, maintenance of a healthy body weight, and psychosocial benefits. WHO recommends for adolescents to accumulate at least 60 minutes of moderate to vigorous intensity physical activity on average per day across the week, which may include play, games, sports, but also activity for transportation (such as cycling and walking), or physical education.Globally, only 1 in 5 adolescents are estimated to meet these guidelines. Prevalence of inactivity is high across all WHO regions, and higher in female adolescents as compared to male adolescents.
To increase activity levels, countries, societies and communities need to create safe and enabling environments and opportunities for physical activity for all adolescents.
Heart disease is a general term that includes many types of heart problems. It's also called cardiovascular disease, which means heart and blood vessel disease.Heart disease is the leading cause of death in the United States, but there are ways to prevent and manage many types of heart disease.
TYPES
There are many different types of heart disease. Some you may be born with, called congenital heart disease. Other types develop during your lifetime.Coronary artery disease (also called coronary heart disease) is the most common type of heart disease. It happens slowly over time when a sticky substance called plaque builds up in the arteries that supply your heart muscle with blood. The plaque narrows or blocks blood flow to the heart muscle and can lead to other heart problems:
• Angina - chest pain from lack of blood flow
• Heart attacks - when part of the heart muscle dies from loss of blood flow
• Heart failure - when your heart can't pump enough blood to meet your body's needs
• Arrhythmia - a problem with the rate or rhythm of your heartbeat
Other types of heart diseases may affect your heart valves or heart muscle (cardiomyopathy).
CAUSES
The causes of heart disease depend on the type of disease. Some possible causes include lifestyle, genetics, infections, medicines, and other diseases.RISK GROUPS
There are many different factors that can make you more likely to develop heart disease. Some of these factors you can change, but others you cannot.• Age. Your risk of heart disease goes up as you get older.
• Sex. Some factors may affect heart disease risk differently in women than in men.
• Family history and genetics. A family history of early heart disease raises your risk of heart disease. And research has shown that some genes are linked to a higher risk of certain heart diseases.
• Race/ethnicity. Certain groups have higher risks than others.
• Lifestyle habits. Over time, unhealthy lifestyle habits can raise your risk heart disease:
• Eating a diet high in saturated fats, refined carbohydrates, and salt.
• Not getting enough physical activity.
• Drinking too much alcohol.
• Smoking and exposure to secondhand smoke
• Too much stress
• Having other medical conditions can raise your risk of heart diseases. These conditions include:
• High blood pressure
• High cholesterol levels.
• Diabetes
• Obesity.
• Autoimmune and inflammatory diseases.
• Chronic kidney disease.
• Metabolic syndrome.
INCIDENCE
Cardiovascular diseases (CVDs) have collectively remained the leading causes of death worldwide and substantially contribute to loss of health and excess health system costs. The Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study has tracked trends in death and disability since 1990 and has provided an updated perspective on the status of cardiovascular health globally, regionally, and nationally.The GBD Study also measures the burden of disease attributable to 88 risk factors for disease. While understanding the underlying physiologic causes of death is important, rigorously evaluating upstream drivers of disease provides additional strategies to guide public policy. These "actual causes of death" reflect modifiable, nongenetic risk factors that cause these diseases. Their role can be estimated by accounting for risk factor prevalence and exposure, strength of relative risk associations with health outcomes, and cause-specific mortality.With this awareness at the forefront, the Global Burden of Cardiovascular Diseases Collaboration, an alliance between the Institute for Health Metrics and Evaluation, the National Heart, Lung, and Blood Institute, and the Journal of the American College of Cardiology (JACC), was launched in 2020. Since then, this collaboration has delivered publications as well as a 5-part region-specific digital series, focused on East Asia, North America, South America, Sub-Saharan Africa, and Western Europe, highlighting their distinct epidemiology. Knowing that the global cardiovascular clinical and research communities desire these data with more frequency, it is our intent to publish results annually .
PREVALANCE
Heart disease is the leading cause of death for men, women, people aged 45 and over, and most race and Hispanic-origin groups The age-adjusted prevalence of heart disease in adults aged 18 and over decreased from 6.2% in 2009 to 5.5% in 2018. In 2019, 5.5% of adults reported that they had been diagnosed with heart disease.From 2009 to 2019, men were more likely than women to report having heart disease.
Leading Modifiable Global Cardiovascular Risk Factors
The Study has produced estimates for the following leading environmental, metabolic, and behavioral risks for CVDs: ambient particulate matter air pollution, household air pollution from solid fuels, lead exposure, low or high temperature, high systolic blood pressure, high low-density lipoprotein cholesterol (LDL-C), high body mass index (BMI), high fasting plasma glucose, kidney dysfunction, dietary risks, tobacco smoking, secondhand tobacco smoke, high alcohol use, and low physical activity
High blood pressure
High systolic blood pressure remains the leading modifiable risk factor globally for attributable premature cardiovascular deaths, accounting for 10.8 million cardiovascular deaths and 11.3 million deaths overall in 2021, and has been particularly linked to ischemic heart disease and stroke-related deaths. Randomized clinical trials have established that more intensive blood pressure targets reduced cardiovascular events compared with more conventional or standard blood pressure control in middle-aged and older adults. More modest blood pressure control is incrementally beneficial even among adults aged ≥80 years. Blood pressure lowering appears to be a particularly important strategy to delay progression to incident heart failure in at-risk individuals. Intensive blood pressure control is projected to extend life expectancy by up to 3 years when initiated in middle age, and antihypertensive treatment optimization appears cost effective at common willing-to-pay threshold Taken together, these data underscore the importance of public health strategies to promote early screening, detection, and treatment of hypertension. Even after diagnosis, traditional step-wise sequencing of prescribing pharmacotherapies may lead to treatment inertia and slow early effective blood pressure control. Simplification of strategies of blood pressure control may improve its implementation in practice and facilitate generalizabilityIn light of existing inequities and unequal access to care, alongside pharmacological approaches, public health measures may be needed to affect population-level blood pressure control. Community-based interventions, including pharmacist-led management and health promotion delivered at barbershops and beauty salons, represent successful and highly cost-effective strategies to address health inequities in blood pressure control. With an aging and expanding global population, the number of people living with suboptimal blood pressure control is increasing.
Dietary risks
Dietary risks accounted for 6.58 cardiovascular deaths and 8 million deaths overall in 2021. This estimate included food types that are underconsumed globally (fruits, vegetables, legumes, whole grains, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids from seafood, and polyunsaturated fatty acids) or overconsumed (red meat, processed meat, sugar-sweetened beverages, trans-fatty acids, and sodium). In 2021, the all-cause DALYs due to dietary risks were 2,340 per 100,000 Excess dietary sodium is a major driver of hypertension in many countries, and modest dietary sodium restriction by 3 grams/day has been projected to avert cardiovascular events and reduce deaths in a cost-saving manner, with benefits projected in all population segments. A report from the Health and Medicine Division of National Academies of Sciences, Engineering, and Medicine identified that reductions in lowering of sodium content in the food supply was a critical step to reaching dietary intake goals. Consumption of sugar-sweetened beverages has been rapidly increasing in recent years, and has been closely linked with adverse weight trajectories, poor nutrition, and higher risks of cardiometabolic illness. Sugar-sweetened beverages are directly marketed toward children and adolescents, and are consumed in high density in areas of poverty and greater food insecurity. Taxation of sugared beverages has been proposed and implemented in various countries, which has been projected to reduce calorie consumption and body weight..High LDL-C
Elevated LDL-C has persisted as a leading modifiable risk factor and is one of the most closely linked markers of atherosclerotic CVD. In 2021, 3.81 million cardiovascular deaths and 3.81 million) deaths overall were attributed to elevated LDL-C levels. In 2021, the all-cause DALYs due to high LDL-C were 1,090 per 100,000 Exposure to lower cumulative LDL-C levels in young and middle-aged adults has been associated with reduced long-term cardiovascular risk, bringing "cholesterol-years" as a marker of atherosclerotic burden into focus as a target for cardiovascular prevention. Statins have represented the cornerstone of primary and secondary prevention of CVDs. Sequential advances in discovery science have identified other effective classes of lipid-lowering therapies that lower LDL-C and positively affect cardiovascular
Air pollution
Air pollution in the forms of ambient particulate matter with an aerodynamic diameter smaller than 2.5 μm) and household air pollution (HAP) from cooking fuels represents the leading environmental risk factor for premature CVD and mortality. In 2021, 4.75 million cardiovascular deaths and 8.54 million deaths overall were attributable to air pollution. In 2021, the all-cause DALYs due to air pollution were 2,990 per 100,000 Heavy PM2pollution events have been closely linked with near-term risks of acute cardiovascular hospitalizations in a dose-dependent and duration-dependent manner
Tobacco
Tobacco is the fifth leading actual cause of cardiovascular death, The WHO target has been set to reduce the prevalence of tobacco smoking by one-third by 2025, and its achievement is projected to prevent a significant number of attributable and preventable deaths to tobacco. impllementation of the WHO MPOWER program, a suite of 6 data-driven strategies (monitoring use, protecting people, offering help, warning, enforcing bans, and raising taxes), has empirically been associated with lower tobacco use. Comprehensive tobacco control programs have been implemented worldwide incorporating price and nonprice interventions that have successfully promoted smoking cessation, reduced per-person consumption, and reduced new initiation.
High body mass index
Obesity is highly prevalent worldwide, closely associated with multiple health risks, and directly contributes to the pathogenesis and progression of CVD. Glucagon-like peptide-1 receptor agonists and dual incretin agonists represent safe and effective options to reduce body weight and potentially protect the cardiovascular system, a hypothesis that is currently being tested. Metabolic surgery has similarly matured to afford substantial weight loss that is durable over time and may have ancillary health benefits including improved glycemic control and remission of diabetes in some. Yet, in most global settings, the prevention and treatment of obesity centers on lifestyle modification, dietary interventions, and improvements in physical activity. Large-scale population-based prevention efforts are needed to construct an environment conducive to healthy behaviors, as has been done previously in the Finnish North Karelia Project Similarly, community-based health promotion and intensive lifestyle management interventions may have durable impact on cardiometabolic health long-term; for instance, the Diabetes Prevention Program has been shown to have "legacy" effects in preventing diabetes even after 20 year Early, comprehensive programs, such as the SI! Program, that can be embedded in schools, have been demonstrated to influence childhood behaviors and cardiovascular health trajectories. High fasting plasma glucose
High fasting glucose tracks closely with high burden of prediabetes, diabetes, and obesity worldwide. In 2021, 2.30 million cardiovascular deaths and 5.4 million deaths overall were attributable to elevated fasting plasma glucose. In 2021, the all-cause DALYs due to high fasting plasma glucose were 1,910 per 100,000 Population strategies to improve glycemic risk overlap substantially with approaches to other primary risk factors including low physical activity and adverse dietary profiles. Scientific progress over the last decade has identified 2 disease-modifying therapeutic classes (the sodium-glucose co-transporter-2 [SGLT-2] inhibitors and the glucagon-like peptide-1 receptor agonists) that prevent cardiovascular complications and kidney disease progression in patients with diabetes. In addition, continuous glucose monitoring has been introduced to minimize glycemic excursions and improve precision of glycemic control. Dissemination and integration of these tools and therapies have been misaligned with risk, giving rise to a "treatment-risk paradox" in which high-risk older persons, Black individuals, or those who are uninsured or underinsured are less likely to be treated with evidence-based therapies.
Kidney dysfunction
Patients who ultimately progress to end-stage kidney disease requiring dialysis face reduced health-related quality of life and heightened risk of death while contributing substantially to increased health system costs. Unfortunately, a large number of people do not have access to necessary renal replacement therapy, with amplified treatment gaps in low- and middle-income countries.62 CVD is the most frequent mode of death, even in the large proportion of patients with earlier stages of chronic kidney disease (CKD). In those with established CKD especially in the presence of proteinuria, the use of renin-angiotensin system inhibitors, SGLT-2 inhibitors, and the nonsteroidal mineralocorticoid receptor agonist finerenone has been shown to not only reduce risk of kidney disease progression but also lower rates of cardiovascular events in this population. The SGLT-2 inhibitor dapagliflozin was shown to be the first therapy to reduce risk of death in patients living with CKD Expanding global access to highly effective pharmacotherapies for CKD remains a substantial challenge.
Lead
Lead exposure remains a silent but major contributor to CVD mortality and health loss. Lead is an underrecognized environmental factor that is linked with hypertension, stroke, coronary artery disease, peripheral artery disease, and other CVDs. In fact, they estimated that as much as 6% to 46% of the decreased CVD-related mortality rate from 1999 to 2014 could be attributable to reductions in blood lead levels.67 There is biological plausibility for the association of lead exposure, blood lead levels, and adverse CVD outcomes. Underlying mechanisms may include derangements in blood pressure and lipid levels, and telomere shortening, even at low blood levels of lead.68 Comprehensive programs to reduce the adverse risks associated with lead exposure have been projected to avert CVDs.69
Nonoptimal temperatures
Nonoptimal ambient temperatures are important contributors to global, regional, and national mortality burdens. Although widespread attention is often paid to the mortality burden of extreme cold or hot temperatures, milder but nonoptimal ambient temperatures account for far greater mortality burden. Exposure to nonoptimal temperatures has been linked to cardiovascular deathsGlobal preparedness initiatives are needed to buffer the cardiovascular effects of weather-related temperature extremes. Increased public health attention is needed on nonoptimal temperatures, especially on moderately hot and moderately cold temperatures, in addition to attention on the effects of extreme temperatures. Additionally, continued research is warranted on the mechanisms underlying the regional variation, population susceptibility, and the effect of acclimatization to nonoptimal temperatures and CVD.
Low physical activity
Low physical activity levels represent an important threat to cardiovascular health. The WHO Global Action Plan for Physical Activity put forth a comprehensive set of approaches, together with evaluative and monitoring frameworks to improve physical activity. Mobile health technologies have been effectively harnessed to promote physical activity and minimize sedentary time. In parallel to these individual changes, structural and environmental changes are needed to facilitate greater physical activity in the workplace and during leisure time.
High alcohol use
There is clear evidence of substantial years of life lost and reduction in life expectancy with heavy alcohol use, especially as alcohol consumption exceeds 100 g weekly.74 While data regarding the cardiovascular health effects of low-level or moderate alcohol consumption have been mixed, cardiovascular risks associated with increased blood pressure and arrhythmias are seen with higher alcohol use, and dangerous or binge alcohol use remains common.. The underlying drivers of marked regional and national-level variability in high alcohol use remain incompletely understood. In the United States, the National Institutes of Health has several research initiatives at the basic, clinical, and population-science levels to address the adverse impact of misuse of alcohol across the lifespan.75 Unfortunately, implementation of established interventions targeting excess alcohol intake has declined globally in recent years.
The Global Burden of Cardiovascular Diseases Collaboration is an ongoing effort to increase the quality and availability of evidence for health decisions. The accompanying almanac of data on regional and national CVD and risk-related burden may serve as a new resource for those developing effective strategies for disease prevention. Updated estimates on CVD burden and risk factors can guide allocation and prioritization of resources for research, health care, and public health.
SYMPTOMS
Heart disease describes a range of conditions that affect the heart. Heart diseases include:
• Blood vessel disease, such as coronary artery disease
• Irregular heartbeats (arrhythmias)
• Heart problems you're born with (congenital heart defects)
• Disease of the heart muscle
• Heart valve disease
Heart disease symptoms depend on the type of heart disease.
Symptoms of heart disease in the blood vessels
Coronary artery disease is a common heart condition that affects the major blood vessels that supply the heart muscle. Cholesterol deposits (plaques) in the heart arteries are usually the cause of coronary artery disease. The buildup of these plaques is called atherosclerosis (ath-ur-o-skluh-ROE-sis). Atherosclerosis reduces blood flow to the heart and other parts of the body. It can lead to a heart attack, chest pain (angina) or stroke.Coronary artery disease symptoms may be different for men and women. For instance, men are more likely to have chest pain. Women are more likely to have other symptoms along with chest discomfort, such as shortness of breath, nausea and extreme fatigue.
Symptoms of coronary artery disease can include:
• Chest pain, chest tightness, chest pressure and chest discomfort (angina)
• Shortness of breath
• Pain in the neck, jaw, throat, upper belly area or back
• Pain, numbness, weakness or coldness in the legs or arms if the blood vessels in those body areas are narrowed Heart disease symptoms caused by irregular heartbeats (heart arrhythmias)
The heart may beat too quickly, too slowly or irregularly. Heart arrhythmia symptoms can include:
• Chest pain or discomfort
• Dizziness
• Fainting (syncope) or near fainting
• Fluttering in the chest
• Lightheadedness
• Racing heartbeat (tachycardia)
• Shortness of breath
• Slow heartbeat (bradycardia)
Heart disease symptoms caused by congenital heart defects
Serious congenital heart defects usually are noticed soon after birth. Congenital heart defect symptoms in children could include:
• Pale gray or blue skin or lips (cyanosis)
• Swelling in the legs, belly area or areas around the eyes
• In an infant, shortness of breath during feedings, leading to poor weight gain
Less-serious congenital heart defects are often not diagnosed until later in childhood or during adulthood. Symptoms of congenital heart defects that usually aren't immediately life-threatening include:
• Easily getting short of breath during exercise or activity
• Easily tiring during exercise or activity
• Swelling of the hands, ankles or feet
Heart disease symptoms caused by diseased heart muscle (cardiomyopathy)
Early stages of cardiomyopathy may not cause noticeable symptoms. As the condition worsens, symptoms may include:
• Dizziness, lightheadedness and fainting
• Fatigue
• Feeling short of breath during activity or at rest
• Feeling short of breath at night when trying to sleep or waking up short of breath
• Irregular heartbeats that feel rapid, pounding or fluttering
• Swollen legs, ankles or feet
Heart disease symptoms caused by heart valve problems (valvular heart disease)
The heart has four valves — the aortic, mitral, pulmonary and tricuspid valves. They open and close to move blood through the heart. Many things can damage the heart valves. A heart valve may become narrowed (stenosis), leaky (regurgitation or insufficiency) or close improperly (prolapse).
Valvular heart disease is also called heart valve disease. Depending on which valve isn't working properly, heart valve disease symptoms generally include:
• Chest pain
• Fainting (syncope)
• Fatigue
• Irregular heartbeat
• Shortness of breath
• Swollen feet or ankles
Endocarditis is an infection that affects the heart valves and inner lining of the heart chambers and heart valves (endocardium). Endocarditis symptoms can include:
• Dry or persistent cough
• Fever
• Heartbeat changes
• Shortness of breath
• Skin rashes or unusual spots
• Swelling of the legs or belly area
• Weakness or fatigue
An epidemic is the rapid spread of disease to a large number of hosts in a given population within a short period of time. For example, in meningococcal infections, an attack rate in excess of 15 cases per 100,000 people for two consecutive weeks is considered an epidemic.
Epidemics of infectious disease are generally caused by several factors including a change in the ecology of the host population (e.g., increased stress or increase in the density of a vector species), a genetic change in the pathogen reservoir or the introduction of an emerging pathogen to a host population (by movement of pathogen or host). Generally, an epidemic occurs when host immunity to either an established pathogen or newly emerging novel pathogen is suddenly reduced below that found in the endemic equilibrium and the transmission threshold is exceeded.
An epidemic may be restricted to one location; however, if it spreads to other countries or continents and affects a substantial number of people, it may be termed a pandemic The declaration of an epidemic usually requires a good understanding of a baseline rate of incidence; epidemics for certain diseases, such as influenza, are defined as reaching some defined increase in incidence above this baseline few cases of a very rare disease may be classified as an epidemic, while many cases of a common disease (such as the common cold) would not. An epidemic can cause enormous damage through financial and economic losses in addition to impaired health and loss of life.
The Centers for Disease Control and Prevention defines epidemic broadly: "the occurrence of more cases of disease, injury, or other health condition than expected in a given area or among a specific group of persons during a particular period. Usually, the cases are presumed to have a common cause or to be related to one another in some way (see also outbreakThe terms "epidemic" and "outbreak" have often been used interchangeably.
Pandemics can cause sudden, widespread morbidity and mortality as well as social, political, and economic disruption. The world has endured several notable pandemics, including the Black Death, Spanish flu, and human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS)
There are several changes that may occur in an infectious agent that may trigger an epidemic. These include:
• Increased virulence
• Introduction into a novel setting
• Changes in host susceptibility to the infectious agent
The conditions which govern the outbreak of epidemics include infected food supplies such as contaminated drinking water and the migration of populations of certain animals, such as rats or mosquitoes, which can act as disease vectors.[
Epidemics can be related to seasonality of certain infectious agents. Seasonality may enter into any of the eight key elements of the system: (1) susceptible recruitment via reproduction, (2) transmission, (3) acquired immunity and recovery, (4) waning immunity, (5) natural mortality, (6) symptomatology and pathology (which may be acute or chronic, depending on the disease), (7) disease-induced mortality, and (8) cross-species transmission. Influenza, the common cold, and other infections of the upper respiratory tract, such as sore throat, occur predominantly in the winter. There is another variation, both as regards the number of people affected and the number who die in successive epidemics: the severity of successive epidemics rises and falls over periods of five or ten years.
Types
Common source outbreak
In a common source outbreak epidemic, the affected individuals had an exposure to a common agent. If the exposure is singular and all of the affected individuals develop the disease over a single exposure and incubation course, it can be termed a point source outbreak. If the exposure was continuous or variable, it can be termed a continuous outbreak or intermittent outbreak, respectively.
Propagated outbreak[
In a propagated outbreak, the disease spreads person-to-person. Affected individuals may become independent reservoirs leading to further exposures.
Many epidemics will have characteristics of both common source and propagated outbreaks (sometimes referred to as mixed outbreak) secondary person-to-person spread may occur after a common source exposure or an environmental vector may spread a zoonotic diseases agent
TransmissioN
• Airborne transmission: Airborne transmission is the spread of infection by droplet nuclei or dust in the air. Without the intervention of winds or drafts the distance over which airborne infection takes place is short, say 10 to 20 feet.
• Arthropod transmission: Arthropod transmission takes place by an insect, either mechanically through a contaminated proboscis or feet, or biologically when there is growth or replication of an organism in the arthropod.[
• Biological transmission: Involving a normal biological process, e.g., passing a stage of development of the infecting agent in an intermediate host. Opposite to mechanical transmission.[
• Contact transmission: The disease agent is transferred directly by biting, sucking, chewing or indirectly by inhalation of droplets, drinking of contaminated water, traveling in contaminated vehicles.
• Cyclopropagative transmission: The agent undergoes both development and multiplication in the transmitting vehicle.[citat
• Developmental transmission: The agent undergoes some development in the transmission vehicle.[
• Fecal-oral transmission: The infectious agent is shed by the infected host in feces and acquired by the susceptible host through the ingestion of contaminated material.
• Horizontal transmission: Lateral spread to others in the same group and at the same time; spread to contemporaries.
• Propagative transmission: The agent multiplies in the transmission vehicle.
• Vertical transmission: From one generation to the next, perhaps transovarially or by intrauterine infection of the fetus. Some retroviruses are transmitted in the germline, i.e. their genetic material is integrated into the DNA of either the ovum or sperm
There have been various major infectious diseases with high prevalence worldwide, but they are currently not listed in the above table as epidemics/pandemics due to the lack of definite data, such as time span and death toll.
• Malaria has had multiple documented temporary epidemics in otherwise non-affected or low-prevalence areas, but the vast majority of its deaths are due to its constant prevalence in affected areas. Throughout history, malaria may have killed 50-60 billion people, or about half of all humans that have ever lived.
• Tuberculosis (TB) became epidemicin Europe in the 18th and 19th century, showing a seasonal pattern, and is still taking place globally The morbidity and mortality of TB and HIV/AIDS have been closely linked, known as "TB/HIV syndemic". According to the World Health Organization, approximately 10 million new TB infections occur every year, and 1.5 million people die from it each year – making it the world's top infectious killer However, there is a lack of sources which describe major TB epidemics with definite time spans and death tolls.
• Hepatitis B: According to the World Health Organization, as of 2019 there are about 296 million people living with chronic , with 1.5 million new infections each year. In 2019, hepatitis B caused about 820,000 deaths, mostly from cirrhosisand hepatocelluliar carcinoma (primary liver cancer). In many places of Asia and Africa, hepatitis B has become endemic.[ In addition, a person is sometimes infected with both hepatitis B virus (HBV) and HIV, and this population (about 2.7 million) accounts for about 1% of the total HBV infections.[
• Hepatitis C: According to the World Health Organization, there are approximately 58 million people with chronic hepatitis C, with about 1.5 million new infections occurring per year. In 2019, approximately 290,000 people died from the disease, mostly from cirrhosis and hepatocellular carcinoma . There have been many hepatitis C virus (HCV) epidemics in history.
Impacts
• Pandemics can cause significant, widespread increases in morbidity and mortality and have disproportionately higher mortality impacts on LMICs.
• Pandemics can cause economic damage through multiple channels, including short-term fiscal shocks and longer-term negative shocks to economic growth.
• Individual behavioral changes, such as fear-induced aversion to workplaces and other public gathering places, are a primary cause of negative shocks to economic growth during pandemics.
• Some pandemic mitigation measures can cause significant social and economic disruption.
• In countries with weak institutions and legacies of political instability, pandemics can increase political stresses and tensions. In these contexts, outbreak response measures such as quarantines have sparked violence and tension between states and citizens
Preparation and Prevention
Preparations for an epidemic include having a disease surveillance system; the ability to quickly dispatch emergency workers, especially local-based emergency workers; and a legitimate way to guarantee the safety and health of health workers.
Effective preparations for a response to a pandemic are multi-layered. The first layer is a disease surveillance system. Tanzania, for example, runs a national lab that runs testing for 200 health sites and tracks the spread of infectious diseases. The next layer is the actual response to an emergency. According to U.S.-based columnist Michael Gerson in 2015, only
the U.S. military and NATO have the global capability to respond to such an emergency. Still, despite the most extensive preparatory measures, a fast-spreading pandemic may easily exceed and overwhelm existing health-care resourcesConsequently, early and aggressive mitigation efforts, aimed at the so-called "epidemic curve flattening" need to be taken.[9] Such measures usually consist on non-pharmacological interventions such as social/physical distancing, aggressive contact tracing, "stay-at-home" orders, as well as appropriate personal protective equipment (i.e., masks, gloves, and other physical barriers to spread)
Malnutrition, in all its forms, includes undernutrition (wasting, stunting, underweight), inadequate vitamins or minerals, overweight, obesity, and resulting diet-related noncommunicable diseases.1.9 billion adults are overweight or obese, while 462 million are underweight.Globally in 2020, 149 million children under 5 were estimated to be stunted (too short for age), 45 million were estimated to be wasted (too thin for height), and 38.9 million were overweight or obese.
Around 45% of deaths among children under 5 years of age are linked to undernutrition. These mostly occur in low- and middle-income countries. At the same time, in these same countries, rates of childhood overweight and obesity are rising.
The developmental, economic, social, and medical impacts of the global burden of malnutrition are serious and lasting, for individuals and their families, for communities and for countries.
Malnutrition refers to deficiencies, excesses, or imbalances in a person's intake of energy and/or nutrients. The term malnutrition addresses 3 broad groups of conditions:
• undernutrition, which includes wasting (low weight-for-height), stunting (low height-for-age) and underweight (low weight-for-age);
• micronutrient-related malnutrition, which includes micronutrient deficiencies (a lack of important vitamins and minerals) or micronutrient excess; and
• overweight, obesity and diet-related noncommunicable diseases (such as heart disease, stroke, diabetes and some cancers).
Various forms of malnutrition
Undernutrition
There are 4 broad sub-forms of undernutrition: wasting, stunting, underweight, and deficiencies in vitamins and minerals. Undernutrition makes children in particular much more vulnerable to disease and death.Low weight-for-height is known as wasting. It usually indicates recent and severe weight loss, because a person has not had enough food to eat and/or they have had an infectious disease, such as diarrhoea, which has caused them to lose weight. A young child who is moderately or severely wasted has an increased risk of death, but treatment is possible.
Low height-for-age is known as stunting. It is the result of chronic or recurrent undernutrition, usually associated with poor socioeconomic conditions, poor maternal health and nutrition, frequent illness, and/or inappropriate infant and young child feeding and care in early life. Stunting holds children back from reaching their physical and cognitive potential.
Children with low weight-for-age are known as underweight. A child who is underweight may be stunted, wasted, or both.
Micronutrient-related malnutrition
Inadequacies in intake of vitamins and minerals often referred to as micronutrients, can also be grouped together. Micronutrients enable the body to produce enzymes, hormones, and other substances that are essential for proper growth and development.
Iodine, vitamin A, and iron are the most important in global public health terms; their deficiency represents a major threat to the health and development of populations worldwide, particularly children and pregnant women in low-income countries.
Overweight and obesity
Overweight and obesity is when a person is too heavy for his or her height. Abnormal or excessive fat accumulation can impair health.Body mass index (BMI) is an index of weight-for-height commonly used to classify overweight and obesity. It is defined as a person's weight in kilograms divided by the square of his/her height in meters (kg/m²). In adults, overweight is defined as a BMI of 25 or more, whereas obesity is a BMI of 30 or more.Overweight and obesity result from an imbalance between energy consumed (too much) and energy expended (too little). Globally, people are consuming foods and drinks that are more energy-dense (high in sugars and fats), and engaging in less physical activity.
Deficiency of protein and energy during infancy is one of the most serious problems throughout the world. It leads to clinical syndromes such as Kwashiorkor, Marasmus, and Anemia.
MARASMUS
Marasmus is due to severe of protein and calorie in the diet.It is not due to calorie deficiency alone because marasmic children subsequently develop kwashiorkor. The common signs and symptoms include loss of body weight and failure in weight gain, body fat depletion, muscles are wasted. The marasmic child is characterized with its thin, lean skinny appearance whereas a kwashiorkor child is flabby with edema or swelling in the body.
KWASHIORKOR
Kwashiorkor is a protein deficiency disease, caused due to poor intake of protein or quality protein over a prolonged period of time. Kwashiorkor causes swelling in the body especially in the hands, feet and the face. The hair and skin show characteristic changes – hair may be light colored or depigmented to reddish yellow and fall off in patches and the skin show patches and become flaky and peel off.
Scope of the problem
In 2014, approximately 462 million adults worldwide were underweight, while 1.9 billion were either overweight or obese.In 2016, an estimated 155 million children under the age of 5 years were suffering from stunting, while 41 million were overweight or obese.
Around 45% of deaths among children under 5 years of age are linked to undernutrition. These mostly occur in low- and middle-income countries. At the same time, in these same countries, rates of childhood overweight and obesity are rising.
RISK GROUPS
Every country in the world is affected by one or more forms of malnutrition. Combating malnutrition in all its forms is one of the greatest global health challenges.
Women, infants, children, and adolescents are at particular risk of malnutrition. Optimizing nutrition early in life—including the 1000 days from conception to a child's second birthday—ensures the best possible start in life, with long-term benefits.
Poverty amplifies the risk of, and risks from, malnutrition. People who are poor are more likely to be affected by different forms of malnutrition. Also, malnutrition increases health care costs, reduces productivity, and slows economic growth, which can perpetuate a cycle of poverty and ill-health.
The United Nations Decade of Action on Nutrition
On 1 April 2016, the United Nations (UN) General Assembly proclaimed 2016–2025 the United Nations Decade of Action on Nutrition. The Decade is an unprecedented opportunity for addressing all forms of malnutrition. It sets a concrete timeline for implementation of the commitments made at the Second International Conference on Nutrition (ICN2) to meet a set of global nutrition targets and diet-related NCD targets by 2025, as well as relevant targets in the Agenda for Sustainable Development by 2030—in particular, Sustainable Development Goal (SDG) 2 (end hunger, achieve food security and improved nutrition and promote sustainable agriculture) and SDG 3 (ensure healthy lives and promote wellbeing for all at all ages).
creating sustainable, resilient food systems for healthy diets;
providing social protection and nutrition-related education for all;
aligning health systems to nutrition needs, and providing universal coverage of essential nutrition interventions;
ensuring that trade and investment policies improve nutrition;
building safe and supportive environments for nutrition at all ages; and
strengthening and promoting nutrition governance and accountability, everywhere.
WHO response To MALANUTRITION
WHO aims for a world free of all forms of malnutrition, where all people achieve health and wellbeing. According to the 2016–2025 nutrition strategy, WHO works with Member States and partners towards universal access to effective nutrition interventions and to healthy diets from sustainable and resilient food systems. WHO uses its convening power to help set, align and advocate for priorities and policies that move nutrition forward globally; develops evidence-informed guidance based on robust scientific and ethical frameworks; supports the adoption of guidance and implementation of effective nutrition actions; and monitors and evaluates policy and programme implementation and nutrition outcomes.
This work is framed by the Comprehensive implementation plan on maternal, infant, and young child nutrition, adopted by Member States through a World Health Assembly resolution in 2012. Actions to end malnutrition are also vital for achieving the diet-related targets of the Global action plan for the prevention and control of noncommunicable diseases 2013–2020, the Global strategy for women's, children's, and adolescent's health 2016–2030, and the 2030 Agenda for sustainable development
Most people can go to the grocery store and buy the food they need, but not everyone can get enough healthy food easily. This is called food insecurity, and it can look different for different people. People can face food insecurity for different reasons, such as if they're unemployed, don't make enough money at their job, or have a disability.
Where someone lives also can affect their ability to get food. For example, some urban areas, rural places, and low-income neighborhoods only have convenience stores and small independent stores instead of full-service supermarkets or grocery stores. That typically means higher prices, fewer choices, and less healthy food. And when public transportation is limited, it can be even harder to get enough healthy meals on the table.
Causes of food Insecurity
Food insecurity can stem from many deep-rooted, complex problems in society. For some, it could be a temporary issue, but for others, it could be a long-standing cyclical problem made worse by many factors in society.
Some of the main causes include:
Poverty, low income, or unemployment. Research shows that if your household income is low, you're 2.6 times more likely to be food insecure. That's because other necessary costs like rent, utilities, and clothing use up any available money.
High living costs. Inflation, an economic structure that drives up the price of goods and services in the economy, affects how you're able to purchase the basics of your day-to-day life. For example, the cost increase in rent, utilities and other household bills, quality foods, transportation, and gas affects how much you're able to spend on food for your household.
Living in a food desert. The level of food insecurity differs from state to state and among neighborhoods in a city or town.
If you live in a rural area with low levels of population, and lack access to markets with fresh foods and produce, with mostly only fast-food options around or near you, you might live in a food desert. Your income and race can also play a role in how you're able to access food on a day-to-day basis. Those who live in urban cities can also find themselves in food deserts. That's because downtowns or busy areas may lack supermarkets that carry fresh, energy-dense foods that are affordable for the entire household.
Lack of access to good, affordable health care. High insurance, high health care costs, medical bills, transport to and from hospitals and clinics, and medication costs might put a sizable dent in your food budget. This, in turn, could make your food insecurity worse.
Systemic racism and discrimination. Research has consistently shown that people of color, especially Black and Hispanic people, are more likely to have food insecurity than white people.
That's because in general, people of color face higher barriers to employment, job loss, higher rates of infection, eviction from homes, and harsher punishments from the criminal justice system, compared to white people.
Risk groups of Food Insecurity
Research has found that some groups of people are more likely to have food insecurity than others. That's because certain factors that cause disparities in society – such as race, gender, sexual orientation, lack of job opportunities, and income levels – can make you less able to get quality, nourishing foods.
Those who are most at risk for food insecurity are:
• Young, non-Hispanic Black males
• Middle-aged Black women
• Hispanic people
• LGBTQ adults
• Children whose parents are unemployed or have low incomes
• Households with multiple children
• Single-parent households, especially those led by women
• Women who live alone
• Men who live alone
• People or households with disabilities
• Adults over the age of 60
Health Risks of Food Insecurity
If you can't get the right amount of food, or enough healthy food, you're more likely to have health problems:
Lifelong disease. Adults in low-income, food-insecure conditions are more likely to get chronic diseases, like diabetes, heart disease, or cancer.
Obesity. Adults and children who have food insecurity may be more likely to be obese because they only have access to unhealthy food or they go through cycles of not having enough food, then overeating. Obesity can affect your physical and mental health as well as your social life. It's linked to issues like asthma, depression, diabetes, and high blood pressure.
Children's health. Children who live in food-insecure homes are more likely to get sick, have a harder time recovering from sickness, and go to the hospital more often. And if they don't have the right amount of food, they can also have trouble concentrating in school and may misbehave more or have more emotional problems when they're young.
Pregnancy risks. Not having enough food to eat can make a pregnant woman go into labor too early or have a baby with a low birth weight. It also might raise the odds of birth defects, anemia, and developmental problems
Food insecurity also can make health conditions you already have worse. It can lead to underuse or misuse of medications that cost money. When you skip doses or take less than you should, not only can it make your condition worse, it can land you in the hospital and doctor's office more often, and cause more financial stress.
State of Hunger and Malnutrition
According to FAO, "Food security exists when all people, at all times have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life". Food security has three dimensions: availability, affordability and food absorption. Availability can be improved through raising domestic production, more import and better distribution system. Affordability refers to the ability of a person/household to buy sufficient quantity of nutritious food required for healthy life. It can be ensured by providing better income and employment opportunities to the workforce. Food absorption depends on people's access to safe drinking water, sanitation and hygiene facilities. Poor quality of water and sanitation generate negative externality and affect the food absorption. This dimension of food security is crucial because food absorption not only depends on individual household's water and sanitation conditions but also on the other households' water and sanitation status and overall environment of that place.. Contaminated water, open defecation, lack of personal and food hygiene and improper disposal of solid and liquid wastes are key factors responsible for morbidity among masses. Therefore, economic, social and environmental aspects need serious attention for ensuring an effective food security system.
Supply-Side Challenges
In India, enforcement of right to employment and right to food has significantly improved the food affordability for the poor households. NFSA provides guarantee to 75 percent of rural and 50 percent of urban households to have 300 kgs of cereals (rice/wheat/millet at the rate of Rs 3/2/1 per kg) at the very subsidized prices and MGNREGS ensures 100 days of manual employment annually 6 to each willing rural household. If a rural worker works only two days under the MGNREGS, he/ she can easily purchase 300 kgs cereals from the wages. This indicates that 50 percent of food demand can easily be met through these two rights. We can address the demand-side constraints related to food security through legal entitlements, improvement in livelihood options and better food management system. However, major concerns are how to ensure food availability and food absorption. It is in this context that this paper examines the key supply-side challenges of food security in India. We examine major supply-side challenges in the following points.
Trade off between Food and Fuel
Energy prices affect the food prices in two ways: First, rising prices of petroleum products motivates the government and corporate sector to go for producing bio-fuels. Although, in India, grains are not being used to produce ethanol, however, its possibility in future cannot be ruled out. If you look at the trends in developed countries, you will find that indirect demand for cereals (feed-grains and fuel-grains) is much higher than the direct demand. The increasing production of bio-fuel reduces the global availability of food grains for consumption and thus raises the food prices. For instance, one ton of barley/sorghum/rice/wheat can produce 434 liters of bio-ethanol, while one ton of maize, potato, and sugarcane can generate 428, 131 and 99 liters of ethanol, respectively. Whenever global energy prices increases, conversion of food grains into fuel becomes more profitable. About one-fifth of US maize production is used to produce ethanol...
\
Trade off between Food and Feed
Urbanization, rising income, and changing demographic pattern have raised the demand for high income-elastic and more water-intensive dairy and meat products. Analysis of consumption data done in the preceding section shows that direct consumption of food grains in India has been constantly declining over the period; while consumption of dairy and meat products has increased at the same time. This indicates that more land, water and other resources are moving towards these high value food products. In regard of implication of this dietary diversification on the food security, two points may be relevant to mention. First, more consumption of meat and dairy products means more indirect demand for food grains for animal feed, thus affecting their availability for direct human consumption and raising their prices.. Moreover, rising food grains prices also affect the other needs of poor households. Poor households have to spend a large proportion of their income to buy food and therefore, they may have less money to spend on healthcare and education. Thus, it may not only affect their nutrition level by way of reducing quality and quantity of food but also their non-food essential needs
Trade off between Food and Wood
Another most critical issue in context of food security is diversion of cultivated land towards wood farming. High GDP growth is leading to increase consumption of wood and wood products like furniture, timber, pulp & paper., It is expected that in future more land would be brought under cultivation of poplar trees due to various reasons, including labour shortage, low profitability in crop husbandry, and increasing absentee land owners. left. The gradual shift of farm workers from agriculture to non-agricultural activities may increase more land area under plantation, thus creating supply-side constraint to the food security. Increasing indirect demand for cereals and declining areas under cultivation can create mismatch between supply and demand and generate inflationary pressure and consequently the fiscal burden of food security on the government.
Shrinking Land and Water Resources
Increasing use of land and water resources for non-agricultural purposes is also one the key challenges for the future food security of India. Due to urbanization, industrialization and rising per capita GDP, demand for land and water for non-agricultural uses have been constantly increasing.
Actionable Points
In order to remove the supply-side constraints in food security, the following actionable points can be taken into account.
1. Cost-effective supply of food to the end-users is as critical as its cost-effective production. Therefore, existing delivery mechanism needs to be reformed. Academicians and experts S. P. Singh Journal of Economic & Social Development 11 have suggested several measures, including direct cash transfer and food stamps to improve the PDS system. These measures may be attempted on pilot basis to examine their efficacy. Decentralization of procurement and distribution could be another option. Gram panchayats may be involved to locally procure and distribute food grains to the entitled households twice in a year (Rabi and Kharif seasons). Computerization of records and the issue of smart cards to PDS beneficiaries may improve accountability and transparency in the PDS system.
2. There is need to boost investment in agriculture innovation systems, including technology transfer and farm extension services, rural infrastructure, post-harvesting R&D to reduce waste, etc. Price stability, crop insurance, reform in tenancy and lease laws, promotion of contract farming and incentives to food processing industries are some of the policy-driven factors that may be considered.
3. Water would be the key issue for future food security. Its demand would increase in nonagricultural uses, including household, industry and environmental flow. It is, therefore, necessary to reduce water consumption in agriculture through better technology, management practices and change in cropping pattern. New technologies such as laser land leveling, zero tillage and sprinkler and drip irrigation, etc can be promoted to improve irrigation efficiency. Water credit system in agriculture may be introduced and water literacy among farmers needs to be promoted.
4. Encourage corporate sector to use a part of its CSR funds towards training, skill formation and capacity building of farmers so that they may adopt water efficient, cost-effective and sustainable farming system, including organic farming. Agricultural subsidies be rationalized and at least, one-third of these subsidies can be transferred from chemical fertilizers to biofertilizers and organic nutrients. Moreover, there is need to reorient agriculture R&D, extension and training system towards development and transfer of technology suited to the sustainable agriculture.
5. Invest in drinking water, sanitation, and other public services would help to improve food absorption.
Food insecurity and the lack of access to affordable nutritious food are associated with increased risk for multiple chronic health conditions such as diabetes, obesity, heart disease, mental health disorders and other chronic diseases
Inequalities in health and health care are caused by different factors. Measuring "unfair" inequalities implies that a distinction is introduced between causal variables leading to ethically legitimate inequalities and causal variables leading to ethically illegitimate inequalities. An example of the former could be life-style choices, an example of the latter is social background. We show how to derive measures of unfair inequalities in health and in health care delivery from a structural model of health care and health production: "direct unfairness", linked to the variations in medical expenditures and health in the hypothetical distribution in which all legitimate sources of variation are kept constant; "fairness gap", linked to the differences between the actual distribution and the hypothetical distribution in which all illegitimate sources of variation have been removed. These two approaches are related to the theory of fair allocation. In general they lead to different results. We propose to analyse the resulting distributions with the traditional apparatus of Lorenz curves and inequality measures. We compare our proposal to the more common approach using concentration curves and analyse the relationship with the methods of direct and indirect standardization.
Health Care Provision
Health care includes all services dealing with the diagnosis and treatments of disease, or the
promotion, maintenance and restoration of health including personal and non-personal health services (WHO, 2016). While provision refers to the way inputs such as money, staff, equipment and drugs are combined to allow the delivery of health interventions (WHO, 2016). Generally, the goal of health care provision is to improve health outcomes in the population and to respond to people's expectations, while reducing inequalities in both health and responsiveness (Adams et. al., 2002). As an example, in the provision of health services in Malaysia, there are nine essential functions of public health which cover six core areas of activities: promoting health and equitable health gain, health protection, combating threats to public health, injury prevention, and disease control and food safety, with the aims to reduce disease prevalence and health inequalities of the population in the country (WHO, 2012).
Apart from that, evidence shows that the major impact on equity of health services
particularly regarding their potential to reduce severity is attributable to the strength of primary care resources and services in communities and countries . The provision of a health care system in a country that addresses all the issues of accessibility, affordability, efficiency and quality of care will contribute towards the improvement and rationalizing the equity of health in the population. The healthcare provision in a country has led to a number of equity issues, thus this manuscript will be focusing on equity in relation to health services in urban and rural areas, utilization of health care and health care financing. Apart from that, the related issues of equity in privatization and the roles of governments in achieving equity will also be discussed.
HEALTH CARE SERVICES
Health care service is one of the crucial aspects of health care provision. As mentioned earlier, the ultimate aim is to improve health outcomes and reduce health inequalities.,
There are many inequity issues surrounding the health care services all over the world.
This includes health care inequities between urban and rural areas which results from various
Access to Health Services Between Urban and Rural Area
Accessibility to health services in urban and rural areas remains to be one of the important
issues in health system in its pursuit of equity in service delivery and in the development of a health care system worldwide. In India, physical access is a major barrier to health services for India's rural population The facilities are concentrated in the urban areas as compared to the rural areas where many vulnerable groups tend to be clustered in despite the scarce services. This is exacerbated by the rapid development of the private sectors in urban areas which results in unequal geographical distribution of services. Even if the health services are physically available, this does not ensure equity to the urban andrural population. This is because the cost associated with seeking health services by the rural population may be higher as compared to the urban population.
Similarly, in China, there are isolated geographical locations where 80 percent of the poor
population lives such as in the mountainous areas that serve as physical barriers, limiting them from accessing the basic health care). Tertiary hospitals are located mostly in the cities and only about 55 percent of villages have functioning health stations. Health care cost in China differs between the rural and urban areas, in which the costs in rural areas are much higher than in the urban areas. This is mostly due to the
insurance coverage differences between the urban and rural population. The rural population is largely uninsured. The impact on the increased medical cost is greater in the rural areas because the household income did not grow as quickly as it does ifcompared to the urban areas. Therefore, the inequality of health care cost between the urban and rural population in China has contributed to the inequity to the health care services access.
Quality of Health Services between Urban and Rural Area
The differences between the health services quality in the urban and rural areas will result in the inequity of health services provided. In India, even though the health facilities are provided in both the urban and rural areas, the quality of the services is debatable. It is documented that there is a low competence among both the private and public sectors in urban areas . There are also dissatisfactions with the quality of care in the public sector that leads to patients seeking treatment in the private sector but the quality may still be the same. A study in India's rural areas finds that most private providers are unqualified, with fewer than 40 percent having medical degrees and almost 20 percent with uncompleted medical degrees. Therefore, even when the services are
there, equity in quality is not ensured
Inequitable Resource Allocation between Urban and Rural Area
Another important issue between the urban and rural population is the inequitable resource
allocation. In many countries, the allocation of fund and resources of health care are based on the need of the population and they are geographically distributed The efficient
allocation of resources to the urban and rural areas is important to ensure equity of the population with equal need
In India, there is an imbalance in the allocation of resources between the states. A greater proportion of resources are directed towards urban-based services which
are compounded by the private sector's bias towards higher level curative services and to be centred in wealthier urban areas . Therefore, patients with similar need in the urban and rural area may not have equal opportunity for the health service as a
result of inequitable resource allocation.
Similarly, in China, it was found that allocation of public resource has skewed towards the
urban and tertiary care sectors while public subsidies for rural health care decreased
significantly .
The Intergovernmental Panel on Climate Change (IPCC) states that the increase in global atmospheric concentration of carbon dioxide (CO2) is primarily due to fossil fuel use and, in a smaller but still significant level, to land-use change.
An Inconvenient Truth, a documentary by former United States Vice-President Al Gore, has also drawn public attention to the critical issue of global warming and how the burning of fossil fuels has increased the amount of CO2 in the atmosphere. Global warming can result in many serious alterations to the environment, eventually impacting human health. It can also cause a rise in sea level, leading to the loss of coastal land, a change in precipitation patterns, increased risks of droughts and floods, and threats to biodiversity. The effects are already evident in areas like Nunavut, Canada, where Inuit hunters are facing survival challenges due to the thinning of the ice. Explorer Will Steger gives an account of hunters in the Baffin Island, who are faced with the dilemma of unsafe hunting due to ice loss, risking their lives to get in contact with sea animals.
Besides the visible effects on people's livelihoods, global warming is predicted to have a strong and adverse impact on human health. The populations of countries that have contributed the least to global warming are the most vulnerable to death and diseases brought about by higher temperatures. The coastlines along the Pacific Ocean and the Indian Ocean and in sub-Saharan Africa will be at higher risk of enduring the health effects of climate change.
The World Health Organization (WHO) reports that climate change is responsible for at least 150,000 deaths per year, a number that is expected to double by 2030. The effects of global warming will cause dire health consequences:
Infectious diseases. IPCC predicts that global warming will worsen human health conditions, especially in tropical regions. In places like Africa, an increase in temperature signifies an increase in mosquito populations, thus escalating the risk of malaria, dengue and other insect-borne infections. Other regions are also affected. The United States experienced varying levels of malaria outbreaks; in 2006, the United Kingdom was plagued by an outbreak of legionnaires' diseases -- a bacterial lung infection that scientists attribute to global warming. WHO states that global warming will also cause a major increase in insect-borne diseases in Europe. Countries like Azerbaijan, Tajikistan and Turkey might already be in the danger zone for mosquito-borne malaria. However, the ability to tolerate temperature changes differs from region to region. Richer societies can utilize technological advances; for example, the use of more powerful air conditioners and the construction of houses minimize heat retention. On the other hand, developing countries lack not only the technological know-how, but also the resources and public health systems, required to prevent such outbreaks.
Heatwaves. Prolonged periods of abnormally high temperatures can have serious health effects on vulnerable populations, such as the elderly and the sick. This was already seen during the 2003 heatwave in Europe, which claimed approximately 35,000 lives. In a study by Hadley Center for Climate Prediction and Research in the United Kingdom, scientists using computer models showed how greenhouse gas emissions have increased the likelihood of heatwaves. The most common health effect is hyperthermia or heatstroke that can be fatal if left untreated. IPCC predicts that global warming will lead to hot days, followed by nights of high temperatures.
Loss of agricultural productivity. Global warming can result in droughts that can worsen living conditions, particularly in Africa. The World Wild Fund has reported that climate change can drastically alter rainfall pattern, and risk water and food supplies for millions. The IPCC report estimates that approximately 75 million to 250 million people in Africa will be without adequate water and will face food shortages by 2020, as crop productivity will decline by about 50 per cent. Rising temperatures could also result in food shortages for 130 million people in Asia.
Asthma and other respiratory diseases. People suffering from heart problems are more vulnerable to increased temperatures, especially those living in already warm areas, as their cardiovascular system must work harder to keep their body cool. Hot temperatures increase the ozone concentration, which can damage people's lung tissue and cause complications for asthma patients and those with lung diseases.
Increased global warming can also pose a threat to national security, affecting food security, which, in turn, can lead to resource conflicts. At the UN Security Council debate on energy,
security and climate, British Foreign Secretary Margaret Beckett introduced global warming as a security risk. Despite opposition from many Council members, such as the Russian Federation and China, she argued that the loss of basic needs due to climate change in poor countries can increase the risk of conflicts. Similarly, Ugandan President Yoweri Museveni has labelled climate change as "an act of aggression by the rich against the poor".
On a positive note, many countries have now realized the grave consequences of global warming. The United States Supreme Court ordered the Federal Government to look into regulating CO2 emissions. Protest participants in many American cities like Boston and New York have urged the Government to reduce emissions up to 80 per cent by 2050; some 1,300 protest events have been organized in the United States under the Step It Up 2007 banner. In Sydney, Australia, businesses and homeowners switched off their lights to acknowledge the critical issue of global warming. Likewise, corporations are realizing the need to become environmentally friendly. PepsiCo, a global beverage and snack company, plans to purchase 1 billion kilowatt hours of renewable energy over the next year. However, the major impact on reducing the effects of global warming cannot be made without the commitment of those countries that account for the greatest production of greenhouse gases
HOW WILL GLOBAL WARMING EFFECT THE HUMAN HEALTH AND WELL BEING?
The major public health organizations of the world have said that climate change is a critical public health problem. According to the U.S. National Institute of Environmental Health Sciences, climate change makes many existing diseases and conditions worse, and it helps pests and pathogens spread into new regions. The most vulnerable people—children, the elderly, the poor, and those with health conditions—are at increased risk for climate-related health effects.
Examples of public health risks
• Extreme heat and poor air quality increase complications from underlying heart and respiratory conditions like asthma, renal failure, and pre-term birth, and as temperatures rise, there will be more heat-related illness and deaths in both urban and rural areas.
• Americans will be exposed to more frequent and/or intense extreme weather and climate events that not only threaten their lives and health, but also significantly disrupt health and social services.
o The risk of very large fires has increased and will increase further across California and other parts of the West, directly threatening people's lives and causing severe air pollution across large areas.
o The frequency and intensity of heavy downpours has increased and is likely to increase further, raising the risk of flash flooding.
• Ticks and mosquitos that transmit illnesses like Lyme disease and West Nile virus are likely to increase and spread to new areas in the United States.
• More frequent heavy rain events will likely increase Americans' exposure to water-borne illnesses, including those linked to sewage contamination of drinking water. Recreational waters are likely to experience more outbreaks of aquatic pathogens, including Vibrio bacteria and harmful algal blooms.
• Human-caused climate change also threatens food safety in multiple ways including lowering the nutritional quality of staples like wheat and rice, causing greater accumulation of mercury and other toxins in seafood, and increasing the chance for food-borne pathogens to enter to food supply.
A natural disaster is characterized by the abnormal intensity of a natural agent (flood, mudslide, earthquake, avalanche, drought) when the usual measures to be taken to prevent this damage were not able to prevent their emergence or were not able to be taken.
Weather- and climate-driven natural disasters include
• flooding caused by heavy rains associated with hurricanes and typhoons (tropical cyclones) other intense storms; drought, famine,
• wildfires brought on by heat waves and shifts in precipitation patterns;
• wind-generated devastation caused by tropical cyclones, tornadoes, derechos, and other windstorms;
• damage and loss of life caused by blizzards and heavy snowfalls.
• Earth-driven natural disasters include large volcanic eruptions (which produce lava flows, explosions, toxic gas clouds, ash falls, and pyroclastic flows that damage populated areas) and strong earthquakes (which result from the sudden fracturing of Earth's crust) powerful enough to damage or destroy built-up areas near their origin points.
Some phenomena that produce natural disasters may be caused by a combination of several different forces. For example, landslides (the movement of large masses of rock, debris, and soil downslope) may be caused by rains that saturate the soil on an unstable slope, or they may be triggered by earthquakes. In a similar manner, the buildup of snow on mountain slopes increases the risks of localized avalanches. Tsunamis,
catastrophic ocean waves that can rise as high as 30 metres (about 100 feet) above normal sea level, are produced by submarine earthquakes, underwater or coastal landslides, volcanic eruptions, or meteor or comet impacts
DAMAGES AND DEATH GLOBALLY
The number of deaths from natural disasters also varies by location and the intensity of the event; however, the overall trend points to a decline from several hundreds of thousands of deaths annually during the first half of the 20th century to roughly 45,000 deaths globally each year. The number of deaths also varies widely from year to year, with smaller natural disasters (or natural disasters occurring in areas far from human settlement) killing few and shockingly large disasters producing truly massive losses of life. Some of the most notable catastrophic disasters in history include the Indian Ocean tsunami of 2004 (which killed more than 225,000 people), the Tangshan earthquake of 1976 (which resulted in more than 242,000 deaths), the 2010 Haiti earthquake (which by some estimates may have killed at least 300,000 people), and China's Shaanxi province earthquake of 1556 (which killed more than 800,000 people).Although deaths from natural disasters have decreased overall, people in lower-income countries often suffer disproportionately, because these locations have fewer resources and thus greater vulnerability to the elements and to food insecurity. In contrast, highly developed countries have better infrastructure (for communications, evacuation procedures, the movement of resources, and the delivery of medical services). In addition, high-income countries can implement policies that limit construction in flood-prone areas or mandate the construction of more earthquake-resistant homes, office buildings, and other structures, thereby reducing the risk of crushing injury and death stemming from building collapses. Consequently, relatively few people die from earthquakes in California, a location well-known for its strong building codes with respect to withstanding earthquakes, compared with places such as Iran and Pakistan, where building codes are either less stringent or whose codes frequently go unenforced.
HEALTH IMPACTS
Disasters throughout history have had significant impact on the numbers, health status and life style of populations. It induce: Deaths, Severe injuries, requiring extensive treatments, Increased risk of communicable diseases, Damage to the health facilities, Damage to the water systems, Food shortage, Population movements. The authors focused on the natural disasters, caused by natural forces rather than by acts associated with human behavior and that affect a large population in a widespread geographic region. Describing the general effects of disasters on health, it does not pretend to cover every contingency. Review of recent literature on humanitarian emergencies has shown that the public health consequences of natural disasters are complex. Disasters directly impact the health of the population resulting in physical trauma, acute disease and emotional trauma. In addition, disasters may increase the morbidity and mortality associated with chronic disease and infectious disease through the impact on the health care system.
DEFINITION
Stroke is defined as abrupt onset of a focal neurological deficit lasting more than 24 hours. It is also called cerebrovascular accident (CVA) or apoplexy.
An acute stroke refers to the first 24-hour. Focal neurological deficit lasting less than 24 hours (usually 5–20 minutes) known as transient ischemic attack (TIA).
INCIDENCE
• Stroke remains the second leading cause of death at the global level and in the European region. Of the 56 million deaths that occur every year worldwide, 10.8% are due to stroke
• Eighty-five per cent of these stroke deaths among all ages occur in developing countries.
• Women have a higher lifetime risk of stroke than men: roughly onein five women (20% - 21%) and one in six men (14% - 17%) will suffer a stroke in their lifetime, according to a 2006 study.
• Overall stroke mortality has been declining worldwide despite the increased percentage ofpeople aged over 65 years (75% of stroke victims are above 65 years old. .This is mainly due to decreased exposure to risk factors, mainly hypertension and smoking, and to improved access to better healthcare.
Stroke is one of the leading causes of death and disability in India. The estimated adjusted prevalence rate of stroke range, 84-262/100,000 in rural and 334-424/100,000 in urban areas. The incidence rate is 119-145/100,000 based on the recent population based studies. There is also a wide variation in case fatality rates with the highest being 42% in Kolkata
In Kerala, according to the data of the Trivandrum Stroke Registry at the SCTIMST, the annual incidence of stroke is between 120-140 per 1 lakh population. The mortality rate is approximately 25%
PREVALENCE
• The prevalence of stroke events is expected to increase significantly across the globe as the global population older than 65 years of age, continues to increase by approximately nine million people per year. Europe, the proportion of the population over 65 years of age is expected to increase from 20% in 2000 to 35% in 2050. The number of stroke events in Europe is predicted to rise from 1.1 million in 2000 to 1.5 million per year by 2025, largely due to the ageing population.
• In 2005, the global prevalence of stroke survivors was estimated to be 62 million, with projections to reach 77 million by 2030.23 However, with the increasing prevalence of stroke survivors comes a consequent increase of people who suffer from stroke-related disabilities.
• Stroke is associated with 43.7 million lost DALYs (disability-adjusted life years) annuallyaround the world, which accounts for about 3.2% of all annually lost DALYs.
• Eight to twelve per cent of ischaemic strokes and 37–38% of haemorrhagic strokes result in death within 30 days.24;25 Fifty to seventy per cent of patients who survive an ischaemic stroke will recover functional independence three months after onset, but 20% will require institutional care.
• Inaddition, 2004 estimates predict that stroke will be among the five most important causes of disability in both developing and developed countries.
Stroke is one of the leading causes of death and disability in India. The estimated adjusted prevalence rate of stroke range, 84-262/100,000 in rural and 334-424/100,000 in urban areas. The incidence rate is 119-145/100,000 based on the recent population based studies
CLASSIFICATION
Stroke is classified on the basis of its aetiology as either ischaemic (87%) or haemorrhagic (13%).
• Ischaemic stroke is produced by occlusion of a cerebral artery [thrombotic or atherosclerotic (50%), embolic (25%) and microartery occlusion, "lacunar stroke", (25%)].
• Hemorrhagic stroke is caused mainly by spontaneous rupture of blood vessels or aneurysms or secondary to trauma.
1. Ischemicstroke
Neurological symptoms and signs of an ischaemic stroke usually appear suddenly, but less frequently, they occur in a progressive manner (stroke-in-progress).The typical presentation is the sudden onset of hemiparesis in an older person.
Symptoms and signs vary depending on the location of the occlusion and the extent of the collateral flow.
Atherosclerotic Ischemic stroke is more common in the elderly, and occurs without warning in more than 80% of cases. A TIA a few months before the stroke is considered an important warningsign.
The pathophysiology is similar to that of ischaemic heart disease; an atheroscleroticplaque in a cerebral artery ulcerates triggering the aggregation of platelets and coagulation of fibrin to produce the thrombus that occludes the artery. Fewer than 20% of cases do not evolve to ulceration, but progress to cause gradual obstruction of flowand may manifest as TIAs
In hypertension-induced arteriosclerosis, small penetrating arteries of the deep whitematter of the brain are affected producing small infarctions known as "lacunar infarcts".
Embolic ischaemic stroke is more frequent in patients with atrial fibrillation (80%), myocardial infarction, prosthetic valves, rheumatic heart disease and larger artery atheroma (artery-artery embolus).
Depending on the severity of the ischemia, infarction (cellular death) will occur within minutes, causing irreversible damage even after blood flow is restored. This is called the "core" of the infarct.Surrounding the core is tissue that is affected functionally due to diminished circulation but may recover if blood flow is restored.7 This is called the "ischaemic penumbra" of a stroke.
Most people will have an ischaemic penumbra amenable to treatment for 3 hours, but many patients may have it up to 12 hours. This is known as the 'therapeutic window' available for thrombolysis.
2.Hemorrhagicstroke
There are two types: one resulting from intracerebral haemorrhage secondary to hypertension, cerebral amyloid angiopathy, or degenerative arterial disease; and the other secondary to subarachnoid haemorrhages caused by rupture of an aneurysm.
Most intracerebral haemorrhagic strokes develop over 30–90 min Symptoms will depend on the location and extent of the haemorrhage. Focal neurological symptoms, vomiting and drowsiness are common. Headache may be present, but stiff neck and seizures are uncommon. Large haemorrhages may cause stupor or coma
Most sub-arachnoid hemorrhages appear suddenly with intense headache, vomiting and neurological deficit and altered consciousness may occur in about 50% of patients. Occasionally, prodromal neurological symptoms, such as paralysis of a limb, difficulty in speaking, visual impairment or sudden unexplained headache, appear before a haemorrhage from an enlarging aneurysm causing pressure on the surrounding tissue or as a result of a leak of blood into the subarachnoid space ("warning leaks").
Cerebral vasospasm is an early complication and re-bleeding or hydrocephalus may be complications of SAH in 30% of cases during the first month, resulting in an extra 60% mortality.
Of those who survive, more than half will have significant disabilities. The annual risk of recurrence of bleeding of an aneurysm is 3%. Thus, early surgical or intravascular treatment of aneurysm in these patients improves their long term outcome.
RISK FACTORS
A stroke risk factor is something that increases your chances of developing a stroke. Sometimes the risk is a result of personal choices such as smoking, and other times the risk is from nonmodifiable factors such as age .
A. NON-MODIFIABLE RISK FACTORS
Non-modifiable risk factors include all risk factors for stroke that cannot be affected by individual behaviours. These factors include age, family history, ethnicity, and disorders for which there is no known direct cause.
1.AGE
Age is an important risk factor that cannot be modified. Most individuals who have a stroke are over 65, although the average age of stroke victims continues to decrease. The chance of having a stroke approximately doubles for each decade of life after age 55, and while stroke is more common among the elderly, an increasing number of people under 65 are also having strokes. The mean ages of TIA cases and stroke cases were 50.6 +/- 7.5 years and51.3 +/- 7.6 years respectively.No age is exempt from stroke and when combined with more controllable risk factors suchas hypertension, the combination is more important than age alone.
2.FAMILY HISTORY
Family history has been found to be a factor in ischemic as well as hemorrhagic strokes. Hereditary factors may be genetic, but environmental and learned lifestyles may also play a part. In 1993, the Framingham study searched for a familial link and their results were inconclusive regarding the role of environmental and genetic influences on familial tendencies for strokeSeven years later, a second finding was published on a familial link from the same study. The number of stroke occurrences by that time gave the researchers the statistical power they needed to find a significant association between familial aggregation and stroke.The second Framingham study was able to identify a strong association between parental ischemic stroke and offspring ischemic strokes after adjusting for other factors.
3.HEART DISEASE
Arrhythmias of the heart, valvular disease, previous myocardial infarction, and congenital heart defects are noted as significantly increasing the risk of stroke or transient ischemic attack.Atrial fibrillation alone accounts for up to 15% of the strokes seen in Canada, and this number increases up to one third over the age of 60.
4. ETHNICITY
The American Heart Association (2010) summarizes statistics gathered in the United States where associations between cardiovascular disease and ethnicity have been recorded. In their 2010 statistical update, the report on prevalence by ethnicity shows 1.8% for Asians, 2.7% for Caucasians, 3.6% for Afro-Americans, and 3.9% for American Indians and residents of Alaska (Go et al., 2010). The report goes on to say that the prevalence rates for American Indians are considered unreliable.
B. MODIFIABLE RISK FACTORS
Modifiable risk factors can be controlled or eliminated through lifestyle changes and/or the use of pharmaceutical interventions.
1. HYPERTENSION
Uncontrolled hypertension, defined as blood pressure >140/90 mmHg for an extended period, is an important modifiable risk factor for stroke. Hypertension increases the risk of stroke by two to more than four times, independent of other risk factors .This increased risk is a result of adaptive structural changes in the blood vessels increasing peripheral vascular resistance that may compromise circulation and enhance the risk for ischemic events. Hypertension also increases the risk of intracerebral hemorrhage resulting from damage to the fragile walls of the small arteries inside the deeper areas of the brain. Controlling hypertension long term can result in a 33% decrease in the risk of stroke.Control of hypertension may require lifestyle changes such as increased physical activity, weight loss, alcohol moderation, smoking cessation, lower fat and salt in diets as well as the use of blood pressure lowering medications.
2.DIABETES MELLITUS
The microvascular and macrovascular complications of diabetes create one of the most significant risk factors for ischemic stroke. The Honolulu Heart Program was fundamental in establishing the risk of stroke related to diabetes in a study showed a 2.5 time greater risk of stroke in cases with diabetes, but at that time, it was only a suggestion that the reason for the increased risk was due to atherosclerosis. Chronic high blood glucose was shown to lead to the development of atherosclerosis and subsequently stroke risk. Type II diabetes is preventable and can be controlled in many cases through diet, exercise, medication, and weight control
3.OBESITY
Obesity has been recognized for some time as a contributing factor of hypertension. More recently, it is being examined at least in part as an independent risk factor for STROKE. Findings showed a positive relationship between overweight, obesity and risk of ischemic stroke
independent from age, lifestyle, and other cardiovascular risk factors.The relationship between obesity and stroke was further defined with the results of theINTERSTROKE study that indicated "a much stronger association of stroke risk with waist-to-hip ratio than with body-mass index".
4.SMOKING
Smoking was the strongest predictor of the progression of arterial disease. Smoking is a leading cause of heart disease and is a known risk factor for stroke. Smoking is known to raise triglycerides in blood, damage endothelial cells that line blood vessel walls, cause thickening and narrowing of blood vessels and result in the formation of clots . Further to this, it has been found that inflammatory reactions to smoking are involved in the pathogenesis of atherosclerosis. All the studies found agreed that smoking is a major risk factor for stroke with the Framingham study finding a 30% increase in risk where the MORGAM study found nearly a twofold increase in risk of stroke with smoking. Smoking cessation programs, legislated restrictions and public awareness programs have had a profound effect on attitudes in the last ten years.
5.ALCOHOL
The consumption of alcohol in moderate amounts of 1-2 drinks per day has been associated with a lower risk of ischemic stroke. No cause and effect relationship has been established between alcohol use and stroke but studies such as The Northern Manhattan Stroke Study have shown correlation between moderate use of alcohol and lower levels of low density lipoproteins (LDL) and lower blood pressures in individuals consuming small regular amounts of alcohol. There was no evidence to indicate an increased risk of ischemic stroke with moderate alcohol consumption however, there is also no evidence for recommendations to be made for nondrinkers to initiate consumption, and heavy drinkers continue to be encouraged to reduce or eliminate their alcohol use
6.DYSLIPIDEMIA
Dyslipidemia is a term used to describe excessive levels of blood cholesterol that create plaque deposits on blood vessel walls. These fatty deposits can occur within the brachiocephalic or internal carotid arteries and cause narrowing of the artery that decreases blood flow to the brain and increases the risk of blockage. More commonly, elevated cholesterol levels are treated medically through the use of statins, a type of medication to reduce low density lipoprotein (LDL) levels .
7. METABOLIC SYNDROME
The risk factors for metabolic syndrome include hypertension, glucose intolerance, dyslipidemiaand abdominal obesity. Of these factors, high blood pressure is considered one of the key components causing a stroke. In combination, these same factors carry an even greater risk making the control of each risk factor even more crucial Combinations of specific risk factors carry a higher risk and have been grouped into a category called metabolic syndrome.This clustering of risk factors serves as a predictor for cardiovascular disease and diabetes, in turn may prove to be a predictor of stroke as well The World Health Organization (WHO) definition of metabolic syndrome requires the presence of diabetes mellitus, impaired glucose tolerance, impaired fasting glucose or insulin resistance and two of;
1) blood pressure greater than 140/90
2) Dyslipidemia with specific limits for triglycerides as well as high and low density lipoproteins for men and women.
3) Central obesity determined by waist circumference
4) Microalbuminuria as found in urine output.
8.SICKLE CELL ANEMIA
Sickle cell anaemia is an autosomal dominant disorder with wide clinical manifestations. It may present with haemolytic anaemia with symptoms.Stroke is more common in homozygous ss disease. It is the common cause of young stroke affecting individuals of age group 20 by 11%. The prevalence of stroke with sickle cell anemia is common in early childhood. Early detection by transcranial Doppler in sickle cell disease patients helps in the primary prevention. The rate of developing stroke is 1% in sickle cell disease patients but individuals with evidence of high blood flow velocity by transcranial Doppler have rate of 10% of developing stroke.
9. PHYSICAL ACTIVITY
Physical activity has a vital role in preventing metabolic complications. The premature death and cardiovascular disease can be prevented by regular physical activity. Stroke prevention can also be made by regular physical activity. According to Copenhagen city heart study and Nurses health study, there is an inverse relationship with the level of physical activity and the incidence of stroke. It is documented that leisure time physical activity reduces the incidence of stroke. The protective effect of physical activity is mainly by its role in controlling or modifying various known risk factors for ischemic stroke such as systemic hypertension, obesity, glucose intolerance and reductions in plasma fibrinogen & platelet activation. In other way physical activity improves HDL concentrations and plasma tissue plasminogen activator activity.
10. HOMOCYSTINEMIA
Many case control studies have showed relationship between the levels of homocystiene and the development of stroke. Elevated homocystiene levels in the body can be reduced by using folic acid, vitamin B6 and B12, but no trials have confirmed.
11 .DRUG ABUSE
Drug abuse increases the incidence of both ischemic and haemorrhagic stroke. The association between drug abuse and stroke risk is observed in a study conducted on lower socioeconomic population. There is a convincing evidence that there is a seven fold increase in the incidence of stroke among drug users.. The mechanism by which it produces stroke is by increasing the blood pressure, haematological and haemostatic abnormalities that leads to increased blood viscosity and vasculitis
12.HYPERCOAGULABILITY
Blood disorders are responsible for 5 to 10% of ischemic stroke with an increased frequency in younger patients. Mutations in Factor V Leiden (havingresistance to activated protein C), deficiencies in Protein C.
Protein S&antithrombin III, and disorders of abnormal platelet function are the major hematological conditions that may lead to cerebrovascular events. Several case control studies have confirmed the relationship between the antiphospholipid antibodies (ApL) and the development of ischemic stroke.
13 .ORAL CONTRACEPTIVE USE
The stroke risk with use of OCPs are mainly dose related. Studies with second generation OCP's containing low levels of oestrogens are associated with decreased risk compared to first generation OCP's. Although many studies reported an increased risk, one study reported a little association between the development of stroke and the use of first, second, third generation oral contraceptive pills. Women having other risk factors other than use of OCP's like cigarette smoking, hypertension, diabetes have migraine are at an increased risk of developing stroke.
ETIOLOGY
EMBOLISM TO THE BRAIN OF CARDIAC OR AORTIC ORIGIN
Embolism to the brain may be arterial or cardiac in origin.Commonly recognized cardiac sources for embolism include atrial fibrillation, sinoatrial disorder, recent acute myocardial infarction (AMI), marantic or subacute bacterial endocarditis, cardiac tumors, and valvular disorders, both native and artificial.
MYOCARDIAL INFARCTION
Stroke is an important complication in patients with AMI, occurring in 1% to 3% of all infarctions and in 2% to 6% of patients with anterior wall infarctions.The majority of strokes after AMI are thought to be embolic, arising from left ventricular wall mural thrombi, but a
number may be atherothrombotic or, in Most strokes occur in the first weeks after the infarct, but some risk for stroke remains for an indefinite time.
Echocardiographic studies have demonstrated that left ventricular mural thrombosis occurs in up to 40% of patients with anterior wall MI, particularly in association with wall motion abnormalities. Mural thrombosis is uncommon with inferior wall MI. Risk factors for left ventricular mural thrombosis are large infarctions, left ventricular dilation, or congestive heart failure. Atrial fibrillation may occur after AMI as an independent risk factor. Bleeding events, including intracerebral bleeding, are an uncommon but serious occurrence in patients treated with long-term oral anticoagulants. The rate for intracranial bleeding in long-term studies is approximately 1% per year. Patients identified as being at high risk for systemic embolism are similar to those at risk for left ventricular mural thrombosis. The presence of left ventricular mural thrombosis increases the risk of stroke.Anticoagulation in the acute phase of MI reduces the risk of left ventricular mural thrombosis.
ATRIAL FIBRILLATION
Cerebral infarction in a patient with atrial fibrillation is presumed to result from embolization of intracardiac thrombi, which most commonly form in the left atrial appendage. Autopsy data indicate that stroke is a possibility throughout the life of persons with a history of atrial fibrillation.
VALVULAR DISEASES
Ischemic stroke is a well known complication of cardiac valvular pathology. Its pathogenesis is generally accepted to be an embolism from the diseased native valve or the prosthetic valve that replaced it .
NATIVE VALVES
Of mitral and aortic valve disorders, rheumatic mitral stenosis is the most common associated with thromboembolism, irrespective of the coexistence of mitral regurgitation. Thrombi associated with mitral stenosis can be found on either the atrial wall or in its appendage. The risk of thromboembolism in rheumatic valve stenosis is related to age and low cardiac output, yet it does not correlate well with left atrial size, mitral calcification, or severity of mitral stenosis.
MITRAL VALVE PROLAPSE
Autopsy series have shown that patients with mitral valve prolapse (MVP) have fibrinous deposits on the valve, endothelial denudation, or annular thrombus at the junction with the atrial wall. Myxomatous and redundant valve leaflets seem to be more prone to production of thromboembolic events. Patients with MVP who are asymptomatic are not necessarily candidates for antithrombotic or anticoagulant agents.
Mitral annulus calcification has been associated with mitral stenosis, mitral regurgitation, conduction abnormalities, arrhythmias, and cardiogenic brain embolism. Identification by echocardiography, irrespective of the coexistence of atrial fibrillation, suggests a twofold increase in risk for stroke.
PROSTHETIC HEART VALVES
Diseased heart valves are replaced with either mechanical or bioprosthetic (tissue) valves. Tissue prosthetic valves are believed to be associated with a smaller risk of thromboembolism than mechanical valves. Mitral valve prostheses are associated with a greater risk of thromboembolism, possibly because of the higher incidence of atrial fibrillation and other thromboembolic risk factors in these patients.
EMBOLISM OF AORTIC ARCH ORIGIN
Complicated atherosclerotic plaques of the aortic arch constitute a source of atherothrombolic or cholesterol embolism. A causal link between brain infarcts and complicated plaques with highly mobile thrombi in the lumen of the aortic arch is likely. Plaques without mobile components might merely be markers for diffuse atherosclerosis.The annual risk of recurrent ischemic stroke may be as high as 12% per year in patients with aortic arch plaques >4 mm; risk of stroke, MI, peripheral embolism, and vascular events is 26% per year.
PATENT FORAMEN OVALE
The diagnosis of a patent foramen ovale may be suspected in any stroke patient. Detection of a patent foramen ovale and a right-to-left (ie, venous-to-arterial) shunt can be appreciated by TEE may show the emergence of echogenic microbubbles in the brain circulation. It is not known if the stroke rate is dependent on characteristics of the patent foramen ovale, eg, size, spontaneous shunting, and shunting with Valsalva maneuver. A concomitant hypercoagulable state may be important. When the patent foramen ovale is large, surgical closure may be an option. Catheter placement of a prosthetic device to block the foramen is in development.
CEREBRAL ISCHEMIA DUE TO PERFUSION FAILURE AND ARTERY TO ARTERY EMBOLISM
Stroke due to perfusion failure occurs with severe stenosis of the carotid and basilar artery, and when there is microstenosis of the small deep arteries, the latter may be a common cause of lacunar infarction. Collateral flow into the region may retard development of tissue liquefaction, and CT scan may show few low-density changes and only slight contrast enhancement. Greatly reduced brain metabolism has been documented by single-photon emission CT (SPECT), positron emission tomography (PET), and diffusion-weighted MRI.
LARGE ARTERY ATHEROSCLEROTIC PLAQUE
The carotid artery system is mostly affected at the common carotid artery bifurcation, the siphon, and the M1 segment of the middle cerebral artery. Along the vertebrobasilar circulation, the first and fourth segments of the vertebral artery and the first segment of the basilar artery are frequently affected.
Artery-to-artery embolism is thought to be the most common cause of cerebral infarction associated with plaques of the large cerebral arteries. Watershed infarcts secondary to the hemodynamic compromise may be less common. In situ thrombosis may occur.
VASCULITIS
Inflammatory conditions can involve the cerebral vasculature. Some, like granulomatous angiitis, are primarily limited to intracranial arteries and arterioles.Others usually—but not always—present with systemic manifestations by the time the effects of cerebral involvement
become clinically evident. Giant cell arteritis, systemic lupus erythematosus, and polyarteritis nodosa are examples of this group.
Stroke of undetermined aetiology – after exclusion of all of the above.In the core area of a stroke, blood flow is so drastically reduced that cells usually cannot recover and subsequently undergo cellular death.The tissue in the region bordering the infarct core, known as the ischaemic penumbra, is less severely affected. This region is rendered functionally silent by reduced blood flow but remains metabolically active. Cells in this area are endangered but not irreversibly damaged. They may undergo apoptosis after several hours or days but if blood flow and oxygen delivery is restored shortly after the onset of stroke, they are potentially recoverable.
Embolic stroke – the most common cause of an embolic stroke is atrial fibrillation.
In the core area of a stroke, blood flow is so drastically reduced that cells usually cannot recover and subsequently undergo cellular death.
The tissue in the region bordering the infarct core, known as the ischaemic penumbra, is less severely affected. This region is rendered functionally silent by reduced blood flow but remains metabolically active. Cells in this area are endangered but not yet irreversibly damaged.
They may undergo apoptosis after several hours or days but if blood flow .
IschaemicCascade
After seconds to minutes of cerebral ischaemia, the ischaemiccascade is initiated. This is a series of biochemical reactions in the brain and other aerobic tissues, which usually goes on for two to three hours, but can last for days, even after normal blood flow returns.The goal of acute stroke therapy is to normalise perfusion and intervene in the cascade of biochemical dysfunction to salvage the penumbra as much and as early as possible. Although it is called a cascade, events are not always linear oxygen delivery is restored shortly after the onset of stroke, they are potentially recoverable.
Important steps of the ischaemic cascade
1. Without adequate blood supply and thus lack of oxygen, brain cells lose their ability to produce energy - particularly adenosine triphosphate (ATP).
2. Cells in the affected area switch to anaerobic metabolism, which leads to a lesser production of ATP but releases a by-product called lactic acid.
3. Lactic acid is an irritant, which has the potential to destroy cells by disruption of the normal acid-base balance in the brain.
4. ATP-reliant ion transport pumps fail, causing the cell membrane to become depolarized; leading to a large influx of ions, including calcium (Ca++), and an efflux of potassium.
5. Intracellular calcium levels become too high and trigger the release of the excitatory amino acid neurotransmitter glutamate.
6. Glutamate stimulates AMPA receptors and Ca++-permeable NMDA receptors, which leads to even more calcium influx into cells.
7. Excess calcium entry overexcites cells and activates proteases (enzymes which digest cell proteins), lipases (enzymes which digest cell membranes) and free radicals formed as a result of the ischaemic cascade in a process called excitotoxicity.
8. As the cell's membrane is broken down by phospholipases, it becomes more permeable, and more ions and harmful chemicals enter the cell.
9. Mitochondria break down, releasing toxins and apoptotic factors into the cell.
10. Cells experience apoptosis.
11. If the cell dies through necrosis, it releases glutamate and toxic chemicals into the environment around it. Toxins poison nearby neurons, and glutamate can overexcite them.
12. The loss of vascular structural integrity results in a breakdown of the protective blood brain barrier and contributes to cerebral oedema, which can cause secondary progression of the brain injury.
CLINICAL FEATURES OF STROKE
Any patient presenting with focal deficit or altered sensorium should be suspected and evaluated for stroke. Sudden onset of any of the following clinical feature may be due to cerebral ischemia.
• Hemiparesis/hemiplegia, monoparesis/monoplegia, or (rarely) quadriparesis
• Hemi sensory defects
• Loss of vision (Monocular or binocular )
• Visual field deficits
• Facial weakness
• Double vision
• Aphasia (sensory or motor)
• Dysarthria
• Ataxia
• Vertigo (usually associated with any other feature)
• Altered level of consciousness
Clinical features can occur alone or combined with two or more features. Establishing the time at which the patient was last seen without stroke symptoms, or last known to be normal, is especially critical when fibrinolytic therapy is an option. There are many factors which are responsible for delay inreaching hospital. Cerebrovascular accident that occurred in sleep may go unnoticed by caregiver or patient.If patient noticed symptoms, on getting up from bed, then the time of onset of stroke is defined as the time at which he was last seen to be free of his current symptoms.
SYMPTOMS OF HAEMORRHAGIC STROKE
A hemorrhagic stroke that occurs inside your brain is also called an intracerebral hemorrhage. Symptoms of an ICH can vary from person to person, but they're almost always present immediately after the stroke occurs.
Symptoms may include:
• Total or limited loss of consciousness
• nausea
• vomiting
• sudden and severe headache
• weakness or numbness in the face, leg, or arm on one side of the body
• seizures
• dizziness
• loss of balance
• problems with speech or swallowing
• confusion or disorientation
SYMPTOMS OF ISCHEMIC STROKE
Most ischemic strokes occur rapidly, over minutes to hours, and immediate
medical care is vital.
The signs of a stroke are:
•Sudden numbness or weakness of the face, arm or leg, especially on
one side of the body
•Sudden confusion
•Sudden trouble speaking
•Sudden trouble seeing in one or both eyes
•Sudden trouble walking
•Sudden dizziness, loss of balance or coordination
•Sudden, severe headache with no known cause
The effects of an acute ischemic stroke may cause additional symptoms in
women including:
• Face, arm or leg pain
• Hiccups or nausea
• Chest pain or palpitations
•Shortness of breath
• Not all symptoms occur with every stroke, and sometimes they go away
and return.
• Some patients experience symptoms that clear up within only a few
minutes, which may be a sign of a transient ischemic attack (TIA). This
is known to be one of the early warning signs of a stroke
Acting F.A.S.T. Is Key for Stroke
• Acting F.A.S.T. can help stroke patients get the treatments they desperately need. The stroke treatments that work best are available only if the stroke is recognized and diagnosed within 3 hours of the first symptoms.
• Stroke patients may not be eligible for these if they don't arrive at the hospital in time.
If you think someone may be having a stroke, act F.A.S.T. and do the following simple test:
F—Face: Ask the person to smile. Does one side of the face droop?
A—Arms: Ask the person to raise both arms. Does one arm drift downward?
S—Speech: Ask the person to repeat a simple phrase. Is the speech slurred
or strange?
T—Time: If you see any of these signs, call 9-1-1 right away.
MEDICAL COMPLICATIONS OF STROKE
Medical complications are believed to be an importantproblem after acute stroke and present potential barriers to optimal recovery. Several previous studies have suggested that complications not only are common, with estimates of frequency ranging from 40% to 96% of patients,1–6but also are related to poor outcome.6 Many of the complications described are potentially preventable or treatable if recognized.
1. NEUROLOGICAL:
• Recurrent stroke- about any episode of new weakness or numbness in arms / legs/ new problem with vision or speech.
• Epileptic seizure.
• Unexplained events-blackouts / funny tums.
2. INFECTION:
• URINARY tract infection – symptoms or positive urine culture.
• Chest infection – auscultatory respiratory crackles & Fever / radiographic evidence / new purulent sputum.
• Other infections-any pyrexial illness lasting for more than 24 hours.
3. COMPLICATIONS OF IMMOBILITY:
• Falls-any document falls regardless of cause ( fall with serious injury that is one that resulted in fracture, radiological investigation, neurological investigation, suturing of wound)
• Pressure sore or skin breaks – any skin break or necrosis resulting from either pressure or trivial trauma.
4. THROMBOEMBOLISM:
• Deep vein thrombosis
• Pulmonary embolism
5. PAIN
• Shoulder pain
• Other pains
6. PSYCHOLOGICAL:
• Depression-low mood considered to interfere with daily activities or require psychiatric intervention.
• Emotional-episodes of crying or laughing that are sudden or unheralded and not under local control.
• Anxiety
• Confusion-cognitive disturbance considered to interfere with
necessary care and rehabilitation.
7. MISCELLANEOUS :
Any documented complication resulting in a specific medical or surgical intervention ( GIT haemorrhage, Constipation, episodes of Cardiac failure, Cardiac arrythmias, and arthritis.
PREVENTION OFSTROKE
1. Primary prevention
2. Secondary prevention
PRIMARY PREVENTION OF STROKE
1. Goal: Primary Stroke prevention aims at reducing the likelihood of having a stroke by either reducing the chances of developing risk factors or controlling various risk factors that increase the chance of having a stroke.
2. Methods of Primary Prevention of Stroke:
A. Mass (population-wide) strategy
B. High Risk Strategy
3. Gaps in Primary Stroke/ cardiovascular disease (CVD) prevention
Lack of awareness
Under usage of population-wide strategies
False reassurance of low risk
Management of blood pressure
Lack of local stroke/CVD prediction algorithms: Most the currently used
CVD/stroke prediction algorithms are based on the Framingham study of a primarily white population of North America, which may not be accurate enough for other racial/ethnic groups.
4.Assessing the Risk of First Stroke:
• An ideal stroke risk assessment tool that is simple, widely applicable and accepted, and takes into account the effects of multiple risk factors does not exist.
• Based on some Indian studies, Framingham Risk Scoring –Cardiovascular Disease (FRS-CVD)may be used to predict risk for stroke over 10-20 years for an individual, subject to further validation in Indian patients with stroke.
• Research is needed to validate risk assessment tools across age sex, and regional groups; to evaluate whether any of the more recently identified risk factors add to the predictive accuracy of existing scales; and to determine whether the use of these scales improves primary stroke prevention.
5. Recommendations
1. Hypertension and diabetes mellitus
2. Tobacco use : Counselling, in combination with drug therapy using nicotine replacement or Bupropion is recommended for active smokers to assist in quitting.
• Abstention from cigarette smoking is recommended for persons who have never smoked.
• Community wide or state-wide bans on smoking in public places are reasonable for reducing the risk of stroke and MI.
3. Atrial Fibrillation:
For patients with valvular AF at high risk for stroke, long-term oral anticoagulant therapy with warfarin at a target INR of 2 to 3 is recommended. For patients with non-valvular AF of > 2 and acceptably low risk for hemorrhagic complications, oral anticoagulants (either vitamin K antagonists or newer anticoagulants) are recommended.
Screening for AF in the primary care setting in patients >65 years of age or persons of any age with irregular pulse followed by ECG as indicated can be useful.
4. Mitral stenosis
Anticoagulation is indicated in patients with mitral stenosis and a prior embolic event, even in sinus rhythm.Anticoagulation is indicated in patients with mitral stenosis and left atrial thrombus.Asymptomatic patients who have >70% stenosis of the internal carotid artery should be referred for evaluation to consider need (or otherwise)of carotid intervention to a centre with risk of peri-procedural stroke, myocardial infarction and death 3%.
5. Sickle Cell Disease (SCD):
Transcranial Doppler (TCD) screening for children with SCD is indicated starting at 2 years of age and continuing annually. Transfusion therapy (target reduction of haemoglobin S, 30%) is effective for reducing stroke risk in those children at elevated risk.
6. Alcohol:
Reduction or elimination of alcohol consumption in heavy drinkers through established screening and counselling strategies is recommended.
A. MASS OR POPULATION STRATEGY
To operationalize this strategy,Population Based Screening has also been launched in 2017 in 100 districts (now expanded to 215 districts) for finding suspected cases of hypertension and diabetes at community level.All women and men over 30 years in the population would be screened. On a fixed day in a week at Village or Sub centre, depending upon the distance/ terrain, the ANM, assisted by the ASHA and members of the Village Health, Sanitation and Nutrition Committee(VHSNC), would screen for hypertension and diabetes, two known risk factors for stroke.
With the launch of Ayushman Bharat in 2018, it is envisaged that all existing Health Sub Centres and Primary Health Centres would be upgraded as Health and Wellness Centres to deliver a comprehensive range of primary health care services. This includes preventive,
promotive, curative and rehabilitative aspects of a wide range of services that encompass care for the entire population. As the Health and Wellness centres are being operationalized, the screening, prevention, control and management of NCDsare being rolled out at HWCs, as a first step to expand the range of services.
Key components include –
1. Population enumeration, community based risk assessment and mobilization for NCD screening by ASHAs at community level.
2. Provision of screening services at HSC/ HSC- HWC and PHC/ PHC- HWC level at the center or at the village level, depending upon the context and availability of suitable venue for screening.
3. Referral of screened individuals to PHC / PHC- HWC for confirmatory
diagnosis and initiation of treatment
4. Regular monthly check up and provision of medicines as per treatment plan at the SHC/ SHC- HWC level
5. Health Promotion to create awareness about risk factors and promote life style Modification
SECONDARY PREVENTION
1. Introduction
This includes measures to reduce the risk of recurrence of stroke in patients who have had TIA or stroke. These guidelines apply to vast majority of patients with TIA or stroke, although some of the recommendations may not be appropriate for those with unusual causes of stroke, like trauma, infections, etc.
2. Risk stratification
All stroke and TIA patients must undergo a risk assessment for recurrent stroke and categorized accordingly by a physician trained in stroke care to initiate appropriate investigations and management strategies.
However, secondary prevention should be addressed at all appropriate healthcare encounters on an ongoing basis following a stroke or transient ischemic attack.
3. Evaluation for modifiable risk factors
Every patient should be evaluated promptly for modifiable risk factors but certainly within one week of onset. This includes:
Hypertension
Diabetes
Dyslipidemia
Lifestyle risk factor - diet, daily sodium intake, exercise, weight, smokingand alcohol
Carotid artery stenosis (for those with non-disabling stroke)
Atrial fibrillation or other arrhythmias
Structural cardiac disease
Obstructive sleep apnoea (OSA)
4. Basic investigations
Basic investigations include:CT brain preferably with CTA or brain MRI with MRA, carotid ultrasound, ECG, Echocardiography,complete blood count, serum electrolytes, creatinine, fasting lipid profile, fasting glucose level, HbA1C, coagulation profile, liver function test.
In selected patients, when basic investigations are inconclusive, Holter monitoring for 24-48 hoursshould be done, especially in suspected arrhythmia cases.
In patients below 45 years of age without apparent cause, additional tests like serum VDRL, HIVand anti-phospholipid antibodies, protein C, S and antithrombin III, antinuclear antibodies, anti-cardio lipid antibodies should be done.
For those investigations not available in district hospitals, patient may be referred to higher centres.
5. Interventions
1. Antiplatelet therapy
All patients with ischemic stroke or TIA should receive antiplatelet therapy or anticoagulation as per indication. Addition of proton pump inhibitor/ H2 receptor blocker should not be routine and should only be considered when there is dyspepsia or other significant risk of gastro-intestinal bleeding with Aspirin.
2. Anticoagulation
Anticoagulation should be started in every patient with atrial fibrillation (valvular or non-valvular) unless contraindicated. Combination of antiplatelet and anticoagulation is not recommended, except in cases of acute coronary syndrome or stent placement. Anticoagulation should be considered for all patients who have ischemic stroke associated with mitral valve disease, prosthetic heart valves, or within 3 months of myocardial infarction.
Anticoagulation should not be used for patients in sinus rhythm (excluding intermittent atrial fibrillation) unless cardiac embolism is suspected.
3.Blood Pressure Lowering
Blood pressure lowering treatment is recommended for all patients with history of TIA or stroke. The benefit extends to persons with or without a history of hypertension.
After acute period is over, an optimal target for stroke patients is 130/80 mmHg, but for patients known to have bilateral severe (>70%) internal carotid artery stenosis, systolic BP of 150 mmHg may be appropriate.
4.Carotid Intervention
Patients with TIA or non-disabling stroke and ipsilateral 70-99% internal carotid artery stenosis (measured by two concordant non-invasive imaging modalities or on a catheter angiogram) should be offered carotidintervention within two weeks of the incident event unless contraindicated
• Carotid intervention is recommended for selected patients with moderate (50-69%) stenosis in symptomatic patients.
• Carotid ultrasound / angiogram should be performed on all patients who would be considered for carotidintervention.
5. Intracranial Atherosclerotic Disease
For patients with moderate stenosis (50-69%) of a major intracranial artery, there is no specific recommendation for use of dual antiplatelets. However, highintensity statin and maintenance of systolic BP around 140 mm of Hg is recommended. Intervention in form of stenting or angioplasty is not recommended in intracranial atherosclerotic disease.
6.Blood Sugar Control
After a TIA or ischemic stroke, all patients should be screened for diabetes with testing of fasting plasma glucose, HbA1C, or an oral glucose tolerance testChoice and timing guided by clinical judgment and recognition that acute illness may temporarily perturb measures of plasma glucose. HbA1C is more accurate than other screening tests in the immediate post event period.
7. Myocardial Infarction
VKA is recommended with target INR of 2-3for three months in acute anterior STEMIwith apical akinesis or dyskinesisbut with no mural thrombus.In case of presence of LA/LV mural thrombus, VKA therapy is recommended for 3 months. Patients should also be under care of a cardiologist.
8. Lipid lowering therapy
All patients with history of TIA or ischemic stroke should be treated with a statin if they have a total cholesterol of > 200 mg%, or LDL cholesterol > 100 mg%.Treatment with high dose statin therapy should be avoided or if used, should be with caution in patients with history of haemorrhagic stroke.
9. Lifestyle measures:
All patients who smoke should be advised to stop smoking and to avoid environmental smoke.All patients who can do regular exercise should be advised to do so for at least 30 minutes each day. They should be advised to start with low intensity exercise and gradually increase to moderate levels (sufficient to become slightly breathless).All patients should be advised yoga,use of low fat dairy products and products based on vegetables, fruits and whole grains and plant oils, and reduce intake of sweets and red meat.Patients' body mass index or waist circumference should be measured, and those who are overweight or obese should be offered advice and support to lose weight.
All patients, but especially those with hypertension, should be advised to reduce their salt intake by not adding extra (table) salt to food, using as little as possible in cooking, and avoiding preserved foods, pickles etc. and choosing low salt foods. All patients should be screened for diabetes and treated to achieve target HbAIC 6.5%.All patients should be screened for OSA/sleep apnoeaand refer to higher centre for treatment.
10.Hyperhomocysteinemia
Supplementation with folate, vitamin B6 and vitamin B12 has shown to reduce homocysteine levels, but there is no high quality evidence demonstrating prevention ofstroke. However, in populations where food is not fortified with folic acid, B vitamins may have a protective role on ischemic stroke
Haemorrhagic Stroke
Mainstay of secondary prevention of intra cerebral hemorrhage (ICH)is control of hypertension.
Those who had ICH, whether hypertensive or amyloid angiopathy or subarachnoid hemorrhage, the blood pressure should becontrolledto the target level of 130-135/80-85 .
DIAGNOSIS
Things will move quickly once you get to the hospital, as your emergency team tries to determine what type of stroke you're having. That means you'll have a CT scan or other imaging test soon after arrival. Doctors also need to rule out other possible causes of your symptoms, such as a brain tumour or a drug reaction.
•A physical exam- Your doctor will do a number of tests you're familiar with, such as listening to your
heart and checking your blood pressure. You'll also have a neurological exam to see how a potential stroke is affecting your nervous system.
• Blood tests- You may have several blood tests, including tests to check how fast your blood clots, whether your blood sugar is too high or low, and whether you have an infection.
• Computerized tomography (CT) scan -A CT scan uses a series of X-rays to create a detailed image of your brain. A CT scan can show bleeding in the brain, an ischemic stroke, a tumor or other conditions. Doctors may inject a dye into your bloodstream to view your blood vessels in your neck and brain in greater detail (computerized tomography angiography).
• Magnetic resonance imaging (MRI)- An MRI uses powerful radio waves and magnets to create a detailed view of your brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiography or magnetic resonance venography).
• Carotid ultrasound - In this test, sound waves create detailed images of the inside of the carotid arteries in your neck. This test shows buildup of fatty deposits (plaques) and blood flow in your carotid arteries.
• Cerebral angiogram- In this uncommonly used test, your doctor inserts a thin, flexible tube (catheter) through a small incision, usually in your groin, and guides it through your major arteries and into your carotid or vertebral artery. Then your doctor injects a dye into your blood vessels to make them visible under X-ray imaging. This procedure gives a detailed view of arteries in your brain and neck.
• Echocardiogram - An echocardiogram uses sound waves to create detailed images of your heart. An echocardiogram can find a source of clots in your heart that may have travelled from your heart to your brain and caused your stroke.
TREATMENT
Emergency treatment for stroke depends on whether you're having an ischemic stroke or a stroke that involves bleeding into the brain (hemorrhagic).
ISCHEMIC STROKE
To treat an ischemic stroke, doctors must quickly restore blood flow to your brain. This may be done with:
• Emergency IV medication- Therapy with drugs that can break up a clot has to be given within 4.5 hours from when symptoms first started if given intravenously. The sooner these drugs are given, the better. Quick treatment not only improves your chances of survival but also may reduce complications.
An IV injection of recombinant tissue plasminogen activator (tPA) — also called alteplase (Activase) — is the gold standard treatment for ischemic stroke. An injection of tPA is usually given through a vein in the arm with the first three hours. Sometimes, tPA can be given up to 4.5 hours after stroke symptoms started.
This drug restores blood flow by dissolving the blood clot causing your stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine if tPA is appropriate for you.
• Emergency endovascular procedures- Doctors sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to significantly improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible:
Medications delivered directly to the brain. Doctors insert a long, thin tube (catheter) through an artery in your groin and thread it to your brain to deliver tPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected tPA, but is still limited.
Removing the clot with a stent retriever. Doctors can use a device attached to a catheter to directly remove the clot from the blocked blood vessel in your brain. This procedure is particularly beneficial for people with large clots that can't be completely dissolved with tPA.
This procedure is often performed in combination with injected tPA.The time window when these procedures can be considered has been expanding due to newer imaging technology. Doctors may order perfusion imaging tests (done with CT or MRI) to help determine how likely it is that someone can benefit from endovascular therapy.
Other procedures
To decrease your risk of having another stroke or transient ischemic attack, your doctor may recommend a procedure to open up an artery that's narrowed by plaque. Options vary depending on your situation, but include:
• Carotid endarterectomy -Carotid arteries are the blood vessels that run along each side of your neck, supplying your brain (carotid arteries) with blood. This surgery removes the plaque blocking a carotid artery, and may reduce your risk of ischemic stroke. A carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions.
• Angioplasty and stents- In an angioplasty, a surgeon threads a catheter to your carotid arteries through an artery in your groin. A balloon is then inflated to expand the narrowed artery. Then a stent can be inserted to support the opened artery.
HEMORRHAGIC STROKE
Emergency treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in your brain caused by the excess fluid. Treatment options include:
• Emergency measures- If you take blood-thinning medications to prevent blood clots, you may be given drugs or transfusions of blood products to counteract the blood thinners' effects. You may also be given drugs to lower the pressure in your brain (intracranial pressure), lower your blood pressure, prevent spasms of your blood vessels and prevent seizures.
• Surgery - If the area of bleeding is large, your doctor may perform surgery to remove the blood and relieve pressure on your brain. Surgery may also be used to repair blood vessel problems associated with hemorrhagic strokes. Your doctor may recommend one of these procedures after a stroke or if an aneurysm, arteriovenous malformation (AVM) or other type of blood vessel problem caused your hemorrhagic stroke:
• Surgical clipping - A surgeon places a tiny clamp at the base of the aneurysm, to stop blood flow to it. This clamp can keep the aneurysm from bursting, or it can keep an aneurysm that has recently hemorrhaged from bleeding again.
• Coiling (endovascular embolization) -Using a catheter inserted into an artery in your groin and guided to your brain, your surgeon will place tiny detachable coils into the aneurysm to fill it. This blocks blood flow into the aneurysm and causes blood to clot.
• Surgical AVM removal - Surgeons may remove a smaller AVM if it's located in an accessible area of your brain. This eliminates the risk of rupture and lowers the risk of hemorrhagic stroke. However, it's not always possible to remove an AVM if it's located deep within the brain, it's large, or its removal would cause too much of an impact on brain function.
• Stereotactic radiosurgery- Using multiple beams of highly focused radiation, stereotactic radiosurgery is an advanced minimally invasive treatment used to repair blood vessel malformation.
